
Ten minutes to save a baby: a narrative review of newborn assessment during first minutes of life and relationship to outcomes
Introduction
The first minutes of life represent the most rapid and complex changes in human physiology. Respiratory, cardiovascular, endocrine, thermoregulatory, and biochemical systems must quickly adapt to the relatively harsh extrauterine environment (1). As the infant takes its first few breaths, pulmonary vasculature resistance falls and foetal lung fluid clears. Massive rises in cortisol and catecholamines drive increases in cardiac output, as the transition from foetal to neonatal circulation begins.
This adaptation ensures the infant sustains homeostasis, now independent from the placenta and mother. Any disruption to this delicate transitional period can cause distress to the newborn infant, and potentially lead to adverse short- and long-term outcomes (2-4). Infants with a torturous transition to extrauterine life requiring resuscitation have an increased risk of guarded outcomes, especially for death and serious neurodevelopmental morbidity (2,4-6). A clinician’s role during the first 10 minutes of life is, therefore, crucial to ensure the infant experiences a ‘smooth landing’ to the outside world, safeguarding them from potentially lifelong adversity.
The International Liaison Committee on Resuscitation (ILCOR) provides best-practice recommendations for the support of the neonate during extrauterine transition (7). Depending upon the infant’s condition, delivery room care ranges from a hands-off approach to invasive resuscitation manoeuvres. At each step, the resuscitation team must synthesise the clinical and biometric information available to them which informs the success of their care. Continual assessment and re-assessment allow targeted therapy to be delivered; for example, positive pressure ventilation (PPV) for persistent bradycardia (heart rate, HR, <100 bpm) (7).
The conundrum one faces is the relationship of these metrics to adverse outcomes.
How does the infant’s status in the delivery room affect them later in life? Are we stabbing blindly in the dark with current methods of assessing the infant’s response to resuscitation?
Many studies correlate the intensity of resuscitation to an increased risk of adverse outcomes (3-6), however, very few explore the effect of assessment on the intensity of delivery resuscitation. Additionally, there is uncertain evidence for the relationship of delivery room assessment to adverse outcomes.
The following review will discuss the routine assessment of the newborn during the first 10 minutes of life, with relationship to outcomes. The synthesis of clinical and biometric data to guide the need for intervention is standard-of-care. However, the question remains—is our assessment accurate and useful to predict and prevent adverse outcomes? We present the following article in accordance with the Narrative Review reporting checklist (available at https://pm.amegroups.com/article/view/10.21037/pm-21-84/rc).
Methods
A broad search of published literature from reputable databases was undertaken to identify relevant evidence for this research question. We scrutinized the reference lists of relevant articles, including systematic reviews, meta-analyses, randomized controlled trials, retrospective studies and previous narrative reviews. The selected articles were critically evaluated by the authors prior to use in this narrative review (Table 1).
Table 1
| Items | Specification |
|---|---|
| Date of Search | May 2021 to November 2021 |
| Databases and other sources searched | PubMed, MEDLINE, Google Scholar, reference lists of relevant articles, others |
| Search terms used | No formal search strategy was employed in this narrative review |
| Timeframe | Literature published up to November 4th, 2021 |
| Inclusion and exclusion criteria | Systematic reviews, meta-analyses, randomized controlled trials, retrospective studies and previous narrative reviews |
Delivery room assessment of the newborn infant
In the first instance, a thorough clinical assessment of the newborn provides the practitioner with vital information about the newborn infant’s condition. International expert recommendations suggest a thorough assessment of the newborn in the delivery room, including clinical and biometric methods (7). This assessment guides the need for active resuscitation or intervention.
Colour
The adequacy of perfusion in the neonate is crudely assessed by the infant’s colour. A blue/cyanotic baby is potentially indicative of a high concentration of deoxygenated haemoglobin, and therefore, hypoxemia (8). At normal body pH and temperature conditions, a newborn with mostly fetal haemoglobin would be expected to appear centrally cyanotic at oxygen saturations of <75–85%. This differs largely from an adult counterpart, who would appear centrally cyanotic at SpO2 <94% (8). Additionally, the characteristics of foetal and adult haemoglobin differ; foetal haemoglobin binds more readily to oxygen, meaning oxygen saturations remain higher at relatively low arterial oxygen tensions (8).
O’Donnell et al. (9) found a profound incongruity between clinicians’ assessment of infants’ colour. There was a wide range of SpO2 at the time-point clinicians believed infants to turn pink, thought to be partially influenced by the resuscitation environment and lighting, to date, no study has examined the effect of neonatal skin tone on the precision of colour assessment in the delivery room. Overall, the reliability of colour assessment, and subsequent correlation to infants’ condition, is poor. The limitations of using colour to assess perfusion or oxygenation in the delivery room must be noted. Instead, the clinician should rely upon more reliable methods of assessment to guide their resuscitation effort.
Oxygen saturation
Pulse oximetry
The measurement of peripheral arterial oxygen saturation (SpO2) using pulse oximetry is a non-invasive tool to assess the oxygenation of the newborn during transition to extrauterine life (10). Pulse oximetry utilises the variable absorbance of light in solutions, as described by the Beer-Lambert law, to measure the proportion of oxygenated haemoglobin in pulsatile arterial blood (11). After illuminating the skin with two known wavelengths of light (660 and 940 nm), a detector allows computation of the SpO2 from the proportion of absorbance, calibrated against standard values (11).
The effective acquisition of SpO2 readings in the delivery room remains logistically and technically difficult. There is conflicting evidence regarding best-practice for SpO2 sensor application in the delivery room (12,13). Whether the sensor should first be applied to the infant or connected to the oximeter remains contested. The results of a meta-analysis are awaited to further inform this practice (14).
The infant’s SpO2 evolves dynamically over the first 10 minutes of life (10,15). Observational studies documenting the transition from the relatively hypoxemic intrauterine environment to the oxygen-rich extrauterine atmosphere have shown that it takes >7 minutes to reach a stable SpO2 >90% (15), and even longer in infants born via caesarean section (16). Dawson et al. (15) used data from 468 infants to develop the standard curves of transitional oximetry, which now anchor international expert recommendations of titrating supplemental oxygen to preductal SpO2 (17). This data informs the 80–85% SpO2 target employed by clinicians internationally (18).
However, the standard SpO2 curves are developed from data of healthy full-term infants born at sea level (15,19) which limits the generalisability of these references to infants with pulmonary pathology, including premature infants, infants with known congenital pathology and infants requiring resuscitation at birth. Additionally, contemporary delivery room practices such as delayed cord clamping (DCC) >30 s have been shown to increase SpO2 during the first five minutes of life in vaginal deliveries of term infants (20). One recent systematic review and meta-analysis demonstrated a decreased risk of death after DCC, however, it is unknown whether this effect was due to initial improvement in oxygenation (21).
Further studies are warranted to scrutinize the current SpO2 targets, which are anchored in observational data from healthy term and late preterm infants who did not require resuscitation in the delivery room. Therefore, emerging research aims to assess: (I) the feasibility of current SpO2 targets in infants requiring resuscitation; (II) the relationship of various SpO2 targets to adverse outcomes.
An individual patient data (IPD) meta-analysis of eight randomised controlled trials (RCT) (22) enrolling infants <32 weeks gestation examined the outcomes related to predetermined SpO2 targets in the delivery room. Only 12% of infants had peripheral oxygen saturations within the target range (80–85% at 5 minutes of life), 46% did not reach the target and 42% exceeded it. Prematurity, low initial FiO2, and low birth weight increased odds of SpO2 outside the acceptable range. In an RCT of infants 24–30 weeks gestation, Dekker et al. (23) demonstrated that infants receiving pure oxygen better-achieved oxygen saturation targets than infants receiving low oxygen (23). This suggests that high initial concentrations of initial oxygen may be advantageous to preterm infants. The feasibility of reaching SpO2 targets in infants of other gestations remains to be studied.
There are no clear guidelines on how fast and at what increment FiO2 should be titrated to achieve current SpO2 targets. The continual adjustment of FiO2 to dynamic SpO2 targets is a complex task even for well-trained resuscitation teams, especially during the first few minutes of life. Using a graphic display of SpO2 targets, coupled with real-time SpO2 data, has been shown to improve the time spent within the target range (24). The effect of using these tools on improving the time spent within target ranges and other outcomes requires further study. The development of technology for the automatic titration of FiO2 to real-time SpO2 data during delivery resuscitation is ongoing (25). Dargaville and colleagues examined an automated oxygen titration system with a rapidly responsive adaptive algorithm for preterm infants receiving non-invasive respiratory support for respiratory insufficiency. In 60 crossover studies in 35 infants, automated oxygen titration resulted in greater target range time [mean (range)% for manual titration = 59% (51–64%) vs. automated = 81% (72–85%)] (26). Adapting this technology will offer an exciting possibility for improving precision in the delivery room care of sick newborn infants.
Near-infrared spectroscopy (NIRS) in delivery room assessment
NIRS is a non-invasive tool for the measurement of regional cerebral oxygen saturation (rScO2) (27). NIRS utilises near-infrared light (700–1,000 nm); these wavelengths easily penetrate the thin skin and bone overlying the neonatal cranial vault. NIR light is absorbed at different wavelengths by oxygenated and de-oxygenated haemoglobin, allowing various detectors to compute the rScO2. The rScO2 provided by NIRS is mostly representative of the venous saturation (75%) (27). The nuances of technicalities surrounding NIRS are beyond the scope of this article; however, they are detailed well in existing literature (28).
Data from 381 neonates have been used to define the reference range for rScO2 immediately after birth. At five minutes, the 10th and 90th centiles were 65% to 90% (median 68%). However, most of these data are from caesarean deliveries, with very few from preterm infants <37 weeks gestation (29). None of these infants received any respiratory support. Katheria et al. assessed the utility of cerebral NIRS to predict adverse neurological outcomes (30). They found that infants with severe intraventricular haemorrhage (IVH) (grade 3–4) or infants who died within 3 days of life had significantly lower cerebral NIRS during the first 10 minutes of life (30). Additional data are needed to further explore this relationship.
Cerebral NIRS is only indicative of oxygenation in the brain, as rScO2 does not necessarily correlate with oxygenation elsewhere in the body. Cerebral autoregulation maintains cerebral blood flow (CBF) despite changes in blood pressure elsewhere in the body (31). Therefore, despite reassuring rScO2, an infant may be hypoxic and/or hypoperfused in other oxygen-sensitive tissues. This significantly limits the utility of NIRS in the delivery room, as it is vital to assess both cerebral and global oxygenation. Additional studies exploring the association between rScO2 and peripheral SpO2 would be useful to further scrutinise the ability of NIRS to detect peripheral hypoxia. NIRS may have a role as an adjunct method of monitoring the neonate’s response to transition, however, given the present body of evidence, NIRS is not yet appropriate for use as the sole method of measuring oxygenation in the delivery room.
Respiratory function monitoring (RFM)
Measurement and surveillance of respiratory function during neonatal resuscitation is an important modality during neonatal resuscitation. RFMs are useful devices that synthesise airway pressure values, flow and tidal volume waves (32). These can be displayed graphically in waveforms, or shown as numeric values [e.g., peak inspiratory pressure (PIP) or positive end-expiratory pressure (PEEP)] (32). The application of these devices includes confirming the correct placement of endotracheal tubes (ETT), assessing for airway obstruction or respiratory rate (32). A survey of training clinicians demonstrated that advanced neonatal trainees found RFM useful in the resuscitation setting (33). Although RFMs are accurate in various gaseous conditions (i.e., temperature changes) (34) and favoured by many clinicians, they are not recommended for routine use in international guidelines (7). A recent multicentre study of infants concluded that RFM usage did not improve the proportion of inflations within a target volume range (35). Additionally, no differences were noted for most clinical outcomes between the RFM visible and not visible groups. Of note, however, the relative risk of IVH was marginally higher in the RFM not visible group (RR 0.71, 95% CI: 0.50 to 1.0, P=0.049). Despite providing objective biometric data to the resuscitation team, there is insufficient evidence to demonstrate that RFM use improves clinical outcomes during neonatal resuscitation.
Measuring diaphragmatic electrical activity
Conventionally, measuring the electrical activity of the diaphragm has been invasive, therefore, limiting its utility in delivery room resuscitation settings (36). Recently, transcutaneous methods of measuring electrical diaphragmatic activity (dEMG) have been developed, inviting the application of this modality to delivery room resuscitation settings. A recent study of preterm infants (mean gestation 28 weeks) found modest correlation between invasive methods of measuring work-of breathing and dEMG (36). In addition to this, dEMG has also been shown to feasibly measure respiratory rate and heart rate (37). However, the accuracy of this application is more sensitive to electrode positioning, and therefore, human error (38). Until more data on the use of dEMG to measure HR are available, HR by dEMG should be interpreted with caution.
Heart rate
An accurate-or inaccurate-heart rate measurement has the potential to greatly influence delivery room practice. Several clinical practice guidelines (7,39) recommend the initiation of PPV if HR remains <100 bpm after initial steps, and chest compressions if HR remains <60 bpm after attempts have been made to establish effective ventilation (7,39). Thus, selecting a reliable method of measuring HR is vital.
Heart rate by auscultation
Expert guidelines recommend the initial assessment of heart rate (HR) by auscultation before the availability of biometric outputs such as HR by oximetry or electrocardiography (ECG) (7,39). Auscultation allows HR to be rapidly detected with reasonable accuracy (median 14 s; IQR 10–18 s) (40), however, the use of auscultation slightly underestimates HR compared to ECG and pulse oximetry (40). Simulation studies have demonstrated poor precision in the clinical assessment of HR (41,42). In a simulated study, Voogdt et al. (42) found that the mean time to auscultate a heart rate varied between 7–17 s and 26–31% of these simulated assessments were found to be inaccurate. 28% of the time these inaccuracies would have influenced management. The majority (78%) of inaccurate assessments were overestimates, potentially causing failure to intervene appropriately (42). In a small (n=26) study of healthy newborn infants, Kamlin et al. noted that clinical assessment by 23 random observers inaccurately and significantly underestimated infant heart rate compared to ECG monitoring by up to 22 beats per min (43). This may be clinically insignificant in a healthy infant not requiring intervention but could impact on the escalation of care for sicker infants e.g., transition to cardiac massage or inotropic drugs. Further assessment of outcomes with routine use of biometric assessment of heart rate in the delivery room is needed.
Biometric assessment of heart rate
Data from RCTs and observational studies suggest that ECG is the most precise and expeditious (44-47). In their pilot study of 40 premature infants, Katheria et al. (45) concluded that ECG produced an HR reading 48 seconds earlier than pulse oximetry. Similar results were produced by Murphy et al. (47) who found ECG had a shorter time to first HR than pulse oximetry {median [IQR] 24 [19, 39] vs. 48 [36, 69]}. Although ECG is the gold-standard to detect HR quickly, there are no studies that demonstrate the use of ECG improves clinical outcomes compared to other HR assessment modalities. The use of ECG may not be readily available in lower resourced settings. Therefore, without robust evidence to demonstrate the association between ECG and improvement in clinical outcomes, clinicians may opt to use an alternate cheaper modality: auscultation. It is important to note the possibility of pulseless electrical activity (PEA)—a form of cardiac arrest not accurately detected by ECG (48). This is an important limitation of ECG in the delivery room, as ECG may provide a heart-rate reading in an infant without cardiac output. Therefore, ECG should not be relied upon as a sole measurement for HR in the delivery room.
There is a smorgasbord of modalities to assess the infant’s overall condition in the delivery room (Figure 1). It is vital that the clinician recognises the strengths and weaknesses of each method (Table 2).
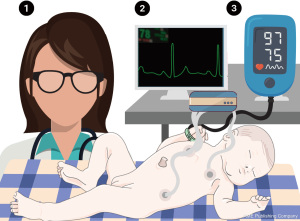
Table 2
| Advantages | Disadvantages | |
|---|---|---|
| Oxygenation | ||
| Colour | • Able to be performed without expensive equipment (available in lower-resourced settings) • Quick assessment modality |
• Confounded by properties of foetal haemoglobin • High inter-clinician variability • Non-precise method of assessment • Unvalidated in infants of various neonatal skin tones |
| Oxygen saturation by pulse oximetry (SpO2) | • Non-invasive • Accurate • Simultaneously provides heart-rate reading |
• Logistically and technically difficult • More research required to explore SpO2 targets • Expensive and may not be readily available in lower-resourced settings |
| Oxygen saturation by cerebral NIRS (rScO2) | • Non-invasive | • Logistically and technically difficult • More research required before widespread implementation • Expensive and may not be readily available in lower-resourced settings • Only indicative of oxygenation in the brain |
| Respiratory function | ||
| Respiratory function monitors (RFM) | • Non-invasive • Accurate despite changes to gas conditions • Graphical/numeric display of key respiratory parameters |
• Limited evidence correlating an improvement to clinical outcomes • More suitable to advanced/experienced staff |
| Transcutaneous diaphragmatic electromyography (dEMG) | • Non-invasive • Can also reliably record respiratory rate and heart rate |
• Expensive and may not be readily available in lower-resourced settings • Sensitive to human error (electrode placement) |
| Heart rate | ||
| Auscultation | • Quick measurement • Able to be performed before establishment of biometric reading |
• Relatively inaccurate • Commonly overestimated à failure to intervene |
| Heart rate by pulse oximetry | • Accurate • Simultaneously provides SpO2 |
• Slower than ECG • Unavailable in lower-resourced settings |
| Hear rate by electrocardiography (ECG) | • “Gold-standard” • Quicker than pulse oxymetry • Accurate |
• No studies demonstrate ECG > PO impacts outcomes • Inaccurate in pulseless electrical activity • Unavailable in lower-resourced settings |
How does delivery room status affect the outcomes of preterm infants?
The infant’s status in the first minutes of life has a profound ability to influence the rest of their life. Population and cohort data have associated an arduous transition to extrauterine life with an increased risk of death and long-term neurological sequelae (2,49-52).
Short-term outcomes
Both poor oxygenation and heart rate in the delivery room have been associated with adverse short-term outcomes. In a retrospective IPD analysis of 8 RCTs, Oei et al. (22) demonstrated the odds of IVH and short-term mortality were significantly higher in infants with poor SpO2 (<80%) at five minutes of life in preterm infants <32 weeks’ gestation. Statistical significance remained for only IVH after accounting for confounders. In a separate IPD analysis of the same 8 RCTs, Kapadia et al. (53) demonstrated that prolonged bradycardia (<100 bpm for ≥2 min) increased the odds of in-hospital mortality (OR 1.6, 95% CI: 1.2–2.5). The duration of bradycardia was positively correlated with the incidence of BPD, IVH, and mortality. If infants had both prolonged bradycardia and failed to reach SpO2 80% by five minutes of life, the odds of in-hospital mortality were increased 18-fold (53).
There is a paucity of evidence for delivery room outcomes of infants of other gestational ages, including moderate-late preterm infants (MLPT) who account for >84% of all preterm births (54) and who are at high risk of respiratory morbidity as well as cognitive and developmental morbidity (55-57). Indeed, there is an urgent need for robust RCTs to further scrutinise the effect of SpO2 in the delivery room across gestations.
Long-term outcomes
Long-term outcomes are regarded as critically important to practitioners when studying resuscitation in the delivery room (18,58). The impact of a few minutes of hyperoxia or hypoxia on the neurodevelopment of survivors remains unclear. In a follow-up of infants recruited to the Resair 2 study (term hypoxic infants randomised to either air or 100% initial oxygen for respiratory support at birth) (59), Saugstad et al. found no significant differences at 18–24 months in survivors for cerebral palsy and/or mental or other delay (air: 10%, 100% oxygen: 7%) (60). However, only 66% of eligible infants were assessed and assessment methods included a combination of parental questionnaires and neurological examinations rather than formal neurodevelopmental testing e.g., Bayley Scale of Infant Development. It must be noted that oxygen concentrations in the Resair study were not titrated and SpO2 was not monitored, which again, limits the generalisability of these outcomes to today’s practice. Unfortunately, due to the overwhelming secular shift to lower oxygen strategies (61), it is unlikely that further evidence from well-designed and sufficiently large RCTs will be generated to inform on this major knowledge gap (62).
There is more information in preterm infants but again, no study is powered sufficiently to examine long-term neurodevelopmental outcomes after resuscitation with higher or lower oxygen strategies. Nevertheless, individual participant data from 543 infants from 3 studies who were randomised to either lower (≤0.3) or higher (≥0.6) initial FiO2 for resuscitation found no difference in risk death and/or disability (difference –0.2%, 95% CI: –7% to 7%, P=0.96) or with cognitive scores <85 (2%, 95% CI: –5% to 9%, P=0.5) (63). However, infants who reached 5-minute SpO2 ≥80% had decreased risk of disability/death (14%, 95% CI: 7% to 21%) and cognitive scores >85 (10%, 3% to 18%, P=0.01), suggesting that oxygenation even within the first 5 minutes of life, is crucial for both short-term (death) and longer-term outcomes and further study is required. Currently, the HiLo (NCT03825835) and the Torpido 3060 (ACTRN12618000879268) aim to recruit >2,500 preterm infants <29 weeks gestation to determine impact of oxygenation during the first few minutes of life on infant mortality and neurodevelopment.
Future directions
To ensure the multitude of infants born requiring resuscitation are subject to evidence-based intervention, future studies must address several knowledge deficits. Best practice for expeditious attainment of pulse oximetry readings remains unknown. The results of a Cochrane review for this question are awaited (14). Additionally, there remains uncertainty surrounding oxygen saturation targets across gestations. It is unknown whether these targets are feasible and appropriate to prevent adverse outcomes. Indeed, additional data are required to further explore pulse oximetry in the delivery room across gestations. Although ECG is the fastest method to attain an HR reading, it is unknown whether its use in the delivery room prevents adverse clinical outcomes. Additional research is warranted. There is a plethora of exciting future research directions for delivery room care of newborn infants. These additional data are urgently required to inform practice to the millions of infants born around the world each year.
Health equity
It is critically important to recognise the issue of health equity in delivery room practice. Many preterm infants are born in lower-resourced settings of neonatal care (54,64), who may not have access to the necessary equipment to provide recommended care. A recent international survey of 21 countries found imbalances in equipment availability between high- and middle-income countries (18). This included oxygen blending equipment, which is necessary to adhere to currently recommended oxygen supplementation strategies for preterm infants (7).
Addressing deficits in equipment availabilities in lower-resourced centres is difficult. Until a time where each delivery worldwide is attended to with all necessary equipment, clinicians should use the equipment that is available to them. In lower-resourced settings, this may be simple clinical assessment modalities only. Health equity and access to appropriate equipment/services must be recognised in future studies of new technologies for the delivery room care of newborns.
Conclusions
What happens to the infant immediately after birth has the potential to influence the course of their life. An effective and precise delivery room assessment allows the clinical team to intervene where appropriate, and to estimate the risk of morbidity and mortality. The strengths and weaknesses of each assessment modality must be noted during this assessment. No single method of assessment alone is reliable. Future studies of delivery room practice must address knowledge deficits to ensure each newborn infant can experience prosperous first minutes of life.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Ola Didrik Saugstad) for the series “Oxygen in the Newborn” published in Pediatric Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://pm.amegroups.com/article/view/10.21037/pm-21-84/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://pm.amegroups.com/article/view/10.21037/pm-21-84/coif). The series “Oxygen in the Newborn” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hillman NH, Kallapur SG, Jobe AH. Physiology of transition from intrauterine to extrauterine life. Clin Perinatol 2012;39:769-83. [Crossref] [PubMed]
- Carlo WA, Askie LM. Chapter 15 - Optimal Oxygenation in Extremely Preterm Infants. In: Bancalari E. editor. The Newborn Lung (Third Edition). Philadelphia: Elsevier, 2019:261-7.
- Bashir A, Bird B, Wu L, et al. Neonatal outcomes based on mode and intensity of delivery room resuscitation. J Perinatol 2017;37:1103-7. [Crossref] [PubMed]
- Jiang S, Lyu Y, Ye XY, et al. Intensity of delivery room resuscitation and neonatal outcomes in infants born at 33 to 36 weeks' gestation. J Perinatol 2016;36:100-5. [Crossref] [PubMed]
- Bajaj M, Natarajan G, Shankaran S, et al. Delivery Room Resuscitation and Short-Term Outcomes in Moderately Preterm Infants. J Pediatr 2018;195:33-38.e2. [Crossref] [PubMed]
- DeMauro SB, Roberts RS, Davis P, et al. Impact of delivery room resuscitation on outcomes up to 18 months in very low birth weight infants. J Pediatr 2011;159:546-50.e1. [Crossref] [PubMed]
- Wyckoff MH, Wyllie J, Aziz K, et al. Neonatal Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2020;142:S185-221. [Crossref] [PubMed]
- Lees MH. Cyanosis of the newborn infant. J Pediatr 1970;77:484-98. [Crossref] [PubMed]
- O'Donnell CP, Kamlin CO, Davis PG, et al. Clinical assessment of infant colour at delivery. Arch Dis Child Fetal Neonatal Ed 2007;92:F465-7. [Crossref] [PubMed]
- Gottimukkala SB, Sotiropoulos JX, Lorente-Pozo S, et al. Oxygen saturation (SpO2) targeting for newborn infants at delivery: Are we reaching for an impossible unknown? Semin Fetal Neonatal Med 2021;26:101220. [Crossref] [PubMed]
- Jubran A. Pulse oximetry. Crit Care 2015;19:272. [Crossref] [PubMed]
- Louis D, Sundaram V, Kumar P. Pulse oximeter sensor application during neonatal resuscitation: a randomized controlled trial. Pediatrics 2014;133:476-82. [Crossref] [PubMed]
- O'Donnell CP, Kamlin CO, Davis PG, et al. Obtaining pulse oximetry data in neonates: a randomised crossover study of sensor application techniques. Arch Dis Child Fetal Neonatal Ed 2005;90:F84-5. [Crossref] [PubMed]
- Louis D, Sundaram V, Kumar P. Pulse oximeter sensor application during neonatal resuscitation: a randomized controlled trial. Pediatrics 2014;133:476-82. [Crossref] [PubMed]
- Dawson JA, Kamlin CO, Vento M, et al. Defining the reference range for oxygen saturation for infants after birth. Pediatrics 2010;125:e1340-7. [Crossref] [PubMed]
- Altuncu E, Ozek E, Bilgen H, et al. Percentiles of oxygen saturations in healthy term newborns in the first minutes of life. Eur J Pediatr 2008;167:687-8. [Crossref] [PubMed]
- Perlman JM, Wyllie J, Kattwinkel J, et al. Neonatal resuscitation: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Pediatrics 2010;126:e1319-44. [Crossref] [PubMed]
- Sotiropoulos JX, Kapadia V, Vento M, et al. Oxygen for the delivery room respiratory support of moderate-to-late preterm infants. An international survey of clinical practice from 21 countries. Acta Paediatr 2021;110:3261-8. [Crossref] [PubMed]
- Mariani G, Dik PB, Ezquer A, et al. Pre-ductal and post-ductal O2 saturation in healthy term neonates after birth. J Pediatr 2007;150:418-21. [Crossref] [PubMed]
- Padilla-Sánchez C, Baixauli-Alacreu S, Cañada-Martínez AJ, et al. Delayed vs Immediate Cord Clamping Changes Oxygen Saturation and Heart Rate Patterns in the First Minutes after Birth. J Pediatr 2020;227:149-156.e1. [Crossref] [PubMed]
- Fogarty M, Osborn DA, Askie L, et al. Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. Am J Obstet Gynecol 2018;218:1-18. [Crossref] [PubMed]
- Oei JL, Finer NN, Saugstad OD, et al. Outcomes of oxygen saturation targeting during delivery room stabilisation of preterm infants. Arch Dis Child Fetal Neonatal Ed 2018;103:F446-54. [Crossref] [PubMed]
- Dekker J, Martherus T, Lopriore E, et al. The Effect of Initial High vs. Low FiO2 on Breathing Effort in Preterm Infants at Birth: A Randomized Controlled Trial. Front Pediatr 2019;7:504. [Crossref] [PubMed]
- Gandhi B, Rich W, Finer N. Achieving targeted pulse oximetry values in preterm infants in the delivery room. J Pediatr 2013;163:412-5. [Crossref] [PubMed]
- Hütten MC, Goos TG, Ophelders D, et al. Fully automated predictive intelligent control of oxygenation (PRICO) in resuscitation and ventilation of preterm lambs. Pediatr Res 2015;78:657-63. [Crossref] [PubMed]
- Dargaville PA, Marshall AP, Ladlow OJ, et al. Automated control of oxygen titration in preterm infants on non-invasive respiratory support. Arch Dis Child Fetal Neonatal Ed 2022;107:39-44. [Crossref] [PubMed]
- Dix LM, van Bel F, Lemmers PM. Monitoring Cerebral Oxygenation in Neonates: An Update. Front Pediatr. 2017;5:46. Erratum in: Front Pediatr 2017;5:160. [Crossref] [PubMed]
- Jöbsis FF. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science 1977;198:1264-7. [Crossref] [PubMed]
- Pichler G, Cheung PY, Aziz K, et al. How to monitor the brain during immediate neonatal transition and resuscitation? A systematic qualitative review of the literature. Neonatology 2014;105:205-10. [Crossref] [PubMed]
- Katheria AC, Harbert MJ, Nagaraj SB, et al. The Neu-Prem Trial: Neuromonitoring of Brains of Infants Born Preterm During Resuscitation-A Prospective Observational Cohort Study. J Pediatr 2018;198:209-13.e3. [Crossref] [PubMed]
- Armstead WM. Cerebral Blood Flow Autoregulation and Dysautoregulation. Anesthesiol Clin 2016;34:465-77. [Crossref] [PubMed]
- Schmölzer GM, Kamlin OC, Dawson JA, et al. Respiratory monitoring of neonatal resuscitation. Arch Dis Child Fetal Neonatal Ed 2010;95:F295-303. [Crossref] [PubMed]
- Milner A, Murthy V, Bhat P, et al. Evaluation of respiratory function monitoring at the resuscitation of prematurely born infants. Eur J Pediatr 2015;174:205-8. [Crossref] [PubMed]
- Verbeek C, van Zanten HA, van Vonderen JJ, et al. Accuracy of currently available neonatal respiratory function monitors for neonatal resuscitation. Eur J Pediatr 2016;175:1065-70. [Crossref] [PubMed]
- van Zanten HA, Kuypers KLAM, van Zwet EW, et al. A multi-centre randomised controlled trial of respiratory function monitoring during stabilisation of very preterm infants at birth. Resuscitation 2021;167:317-25. [Crossref] [PubMed]
- van Leuteren RW, de Waal CG, Hutten GJ, et al. Transcutaneous monitoring of diaphragm activity as a measure of work of breathing in preterm infants. Pediatr Pulmonol 2021;56:1593-600. [Crossref] [PubMed]
- van Leuteren RW, Bekhuis RE, de Waal CG, et al. Diaphragmatic electromyography in preterm infants: The influence of electrode positioning. Pediatr Pulmonol 2020;55:354-9. [Crossref] [PubMed]
- Kraaijenga JV, Hutten GJ, de Jongh FH, et al. Transcutaneous electromyography of the diaphragm: A cardio-respiratory monitor for preterm infants. Pediatr Pulmonol 2015;50:889-95. [Crossref] [PubMed]
Cite this article as: Sotiropoulos JX, Kapadia V, Ramachandran S, Oei JL. Ten minutes to save a baby: a narrative review of newborn assessment during first minutes of life and relationship to outcomes. Pediatr Med 2022;5:31.

