Factors associated to hospital re-admission of infants previously treated for hyperbilirubinemia
Introduction
Neonatal jaundice holds significant morbidity including acute bilirubin encephalopathy and even death (1). Early identification of infants at risk for unconjugated hyperbilirubinemia has been the focus of much research. A 2006 study by Sgro et al., identified an overwhelming incidence of severe neonatal hyperbilirubinemia in Canada requiring admission for phototherapy (2). These findings resulted in several studies investigating methods and criteria for predicting infants at risk for longstanding consequences from delayed or missed treatment (1,3-14). Despite these efforts, failure to identify or monitor hyperbilirubinemia remains a prevalent issue and a leading contributor of medical malpractice claims costs in Canada (15).
Although Canadian and American guidelines have been developed on screening and timing of decision to treat unconjugated hyperbilirubinemia, there is a lack of knowledge on treatment of infants who, after having completed a course of phototherapy for hyperbilirubinemia, re-present to the emergency department (ED) with persistent hyperbilirubinemia.
Our aim was to identify and explain the potential differences between infants with unconjugated hyperbilirubinemia who re-present to the ED at a single center after a course of phototherapy and get re-admitted for hyperbilirubinemia, and those who do not get re-admitted.
We present the following article in accordance with the STROBE reporting checklist (available at https://pm.amegroups.com/article/view/10.21037/pm-21-89/rc).
Methods
Participants and design
We conducted a retrospective study of infants treated for unconjugated hyperbilirubinemia at London Health Sciences Centre (LHSC) from January 2014 to June 2016. LHSC comprises three institutions: University Hospital, Victoria Hospital, and Children’s Hospital in London, Ontario. Infants less than 3 months of age presenting to the ED with jaundice who received in-patient phototherapy for unconjugated hyperbilirubinemia were included. Criteria that could be considered as confounders based on the application of the Canadian Pediatric Society (CPS) Position Statement on Guidelines for detection, management and prevention of hyperbilirubinemia in term and late preterm newborn infants were identified and considered as exclusion criteria (1). One exception to this exclusion criteria was comorbidity of isoimmune hemolytic disease as it was hypothesized to be potentially significant in predicting a need for re-admission for repeat phototherapy.
A database search for infants coded for hyperbilirubinemia or phototherapy was conducted. Initial electronic chart review was used to screen for and exclude infants born <35 weeks gestational age, infants with electronic discharge summaries specifying comorbidities, or other exclusion criteria. A hard copy chart review followed to rule out further exclusion criteria or confounders noted on paper clinical notes. Timing of phototherapy initiation, discontinuation, and bloodwork procedures were deduced from nursing charts and physician orders. Data on infants who re-presented to LHSC within 14 days of discharge were gathered and analyzed for potential predictive factors of re-admission to hospital.
Measures
Data were collected and managed using REDCap (Vanderbilt University, Nashville, TN) (16). Patients with missing or partial data from outside hospitals were recorded as incomplete. Characteristics including sex, age when infant required initial phototherapy, gestational age, birth weight, and weight at admission were gathered. Infant risk level was classified according to CPS guidelines on management of unconjugated hyperbilirubinemia (1). Since patients with potential confounding risk factors (e.g., G6PD deficiency, asphyxia, respiratory distress) were excluded from analysis, all patients were classified as either “low risk” or “medium risk,” which was based on gestational age alone. When a specific cause of hyperbilirubinemia was not included in either clinical notes or discharge summary, the etiology was described as “other”.
Current Canadian guidelines for management of unconjugated hyperbilirubinemia state that therapeutic thresholds for bilirubin level vary based on infant age and risk factors, with lower, medium, and higher risk thresholds (1). Additionally, guidelines state that conventional therapy may still be considered at bilirubin levels 35–50 µmol/L below designated therapeutic thresholds. To determine whether infants were within treatment proximity (i.e., within 35–50 µmol/L of therapeutic threshold) at the time of discharge, we compared their final measured bilirubin level to their age-appropriate therapy threshold corrected for age at discharge.
Statistical analysis
All analyses were conducted using SPSS v25 (IBM Corp., Armonk, NY, USA). Bivariate analyses examined differences between infants re-admitted and those who were not. Mann-Whitney U and chi-square tests were used for continuous and categorical variables, respectively. Statistical significance was defined as P≤0.05. Logistic regression was used to generate models evaluating the performance of significant individual predictors for repeated admission following initial phototherapy treatment.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Western University research ethics board of London Ontario (REB#107955) and individual consent for this retrospective analysis was waived.
Results
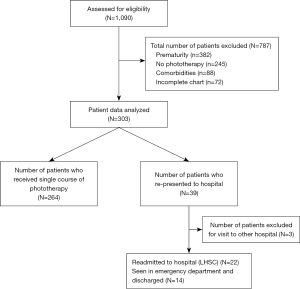
A total of 1,090 patients aged 0–27 days of life were identified from our database search as being coded for either “hyperbilirubinemia” or “phototherapy”. Of these, 787 were excluded due to prematurity, not receiving phototherapy, confounding comorbidities and incomplete charts. A total of 303 patients were assessed for trends in management of hyperbilirubinemia (Figure 1).
Practice trends and variations
Of the 303 included patients, 39 infants re-presented to hospital over concerns of jaundice or feeding within 2 weeks of discharge. Amongst these, 3 infants had a part of their therapy performed at outside hospitals and were therefore excluded. Twenty-two infants required re-admission to LHSC for hyperbilirubinemia management, with 1 infant re-admitted for monitoring and the remainder receiving a second course of phototherapy.
Patient characteristics are shown in Table 1. Based on our selection criteria, no included infants were in the “High Risk” category. The majority of infants requiring phototherapy were diagnosed with breastfeeding failure jaundice (41%), followed by hemolysis (24%) and physiologic jaundice (22%). Phototherapy methods used included bilirubin blankets (61%), single phototherapy (28%) and double phototherapy (26%). No infants required exchange transfusion.
Table 1
| Variable | N (%) | Mean (SD) |
|---|---|---|
| Sex, male | 168 (56.0) | – |
| Average length of stay, days | 300 (100.0) | 3.66 (3.60) |
| Average age at start of initial phototherapy, days | 296 (98.7) | 3.09 (2.46) |
| Gestational age, weeks | ||
| 35–37 | 133 (44.3) | – |
| ≥38 | 155 (51.7) | – |
| >35 but specific gestational age unclear | 12 (4.0) | – |
| Risk stratification | ||
| Low | 133 (44.3) | – |
| Medium | 155 (51.7) | – |
| High | 0 (0.0) | – |
| Unknown | 12 (4.0) | – |
| Weight at admission, grams | 293 (97.7) | 3,079.96 (649.57) |
| Change in weight from discharge | ||
| Weight gain | 125 (41.7) | – |
| Weight loss | 108 (36.0) | – |
| No weight changes | 47 (15.7) | – |
| Unknown | 20 (6.6) | – |
| Etiology of hyperbilirubinemia | ||
| Breastfeeding failure | 123 (41.0) | – |
| Hemolysis | 71 (23.7) | – |
| Physiologic | 66 (22.0) | – |
| Breastmilk | 7 (2.3) | – |
| Hypothyroidism | 0 (0.0) | – |
| Biliary obstruction | 0 (0.0) | – |
| Other | 4 (1.3) | – |
| Type of phototherapy | ||
| Bilirubin blanket | 182 (60.7) | – |
| Single phototherapy | 83 (27.7) | – |
| Double phototherapy | 77 (25.7) | – |
| Triple phototherapy | 37 (12.3) | – |
| Exchange transfusion | 0 (0.0) | – |
| Other | 0 (0.0) | – |
| Unknown | 31 (10.3) | – |
| Re-presented to ED | 36 (12.0) | – |
| Disposition after re-presentation | ||
| Re-admitted to hospital | 22 (7.3) | – |
| Discharged from ED | 14 (4.7) | – |
ED, emergency department; N, number; %, percentage; SD, standard deviation.
Table 2 summarizes demographic data of infants who were re-admitted to hospital for a second course of phototherapy. The majority of infants who did not re-present were treated with bilirubin blankets (62%) with a mean (SD) of 24.5 (20.5) hours of phototherapy treatment as shown in Table 3. On average, 4.67 bilirubin checks were done for each of those infants with 79% having at least one bilirubin check post-discontinuation of phototherapy. One third had checks every 12–24 hours while in hospital and 25% every 8–10 hours.
Table 2
| Demographic characteristics | N (%) | Mean (SD) |
|---|---|---|
| Sex, male | 16 (72.7) | – |
| Age at initial hyperbilirubinemia presentation, days | 20 (90.9) | 2.68 (2.06) |
| Gestational age, weeks | ||
| 35–37 | 12 (54.5) | – |
| ≥38 | 8 (36.4) | – |
| >35 but specific gestational age unclear | 2 (9.1) | – |
| Risk Stratification according to CPS guidelines | ||
| Low | 8 (36.4) | – |
| Medium | 12 (54.5) | – |
| High | 0 (0.0) | – |
| Unknown | 2 (9.1) | – |
| Change in weight from discharge | ||
| Gain | 8 (36.4) | – |
| Loss | 9 (40.9) | – |
| Unknown | 5 (22.7) | – |
| Etiology of hyperbilirubinemia* | ||
| Single etiology | 11 (55.0) | – |
| Multiple etiology | 9 (45.0) | – |
| ABO or other incompatibility | 4 (18.0) | – |
| Type of phototherapy treatment | ||
| Bilirubin blanket only | 2 (9.1) | – |
| Single photopherapy | 5 (22.7) | – |
| Multiple methods | 10 (45.5) | – |
| Unknown | 5 (22.7) | |
| Rebound during initial therapy | 1 (5.0) | – |
| Method of feeding | ||
| Breastfeeding by mouth only | 11 (50.0) | – |
| Multiple methods | 10 (45.5) | – |
| Family history of jaundice | 5 (22.7) | – |
CPS, Canadian Pediatric Society; *, included etiologies of hyperbilirubinemia are shown in Table 1: physiologic jaundice, breastfeeding failure, breastmilk jaundice, hemolysis, hypothyroidism, biliary obstruction and other. N, number; %, percentage; SD, standard deviation.
Table 3
| Patient variables | Single course phototherapy (n=278) | Subsequent re-admission for repeated phototherapy (n=22) | P value | |||
|---|---|---|---|---|---|---|
| N (%) | Mean (SD) | N (%) | Mean (SD) | |||
| Proximity to phototherapy threshold at discharge, µmol/L | – | 102.43 (39.46) | – | 87.92 (35.37) | 0.111 | |
| Bilirubin level at presentation, µmol/L | – | 265.72 (69.60) | – | 232.19 (67.18) | 0.037* | |
| Duration of treatment, hours | – | 24.54 (20.50) | – | 28.84 (31.11) | 0.365 | |
| Average number of bilirubin checks | – | 4.69 (2.83) | – | 4.45 (2.76) | 0.712 | |
| Bilirubin checked post discontinuation | 0.553 | |||||
| No | 12 (4.3) | – | 3 (13.6) | – | ||
| Once | 47 (16.9) | – | 11 (50) | – | ||
| More than once | 129 (46.4) | – | 4 (18.2) | – | ||
| Unknown | 90 (32.4) | – | 4 (18.2) | – | ||
| First bilirubin check after treatment discontinuation, hrs | – | 7.06 (5.69) | – | 8.03 (4.97) | 0.473 | |
| Last bilirubin check after treatment discontinuation, hrs | – | 34.12 (43.16) | – | 32.67 (15.6) | 0.955 | |
| Frequency of bilirubin checks, hrs | 0.297 | |||||
| <6 | 4 (1.4) | – | 0 (0.0) | – | ||
| 6–8 | 36 (12.9) | – | 3 (13.6) | – | ||
| 8–10 | 68 (24.5) | – | 4 (18.2) | – | ||
| 10–12 | 54 (19.4) | – | 2 (9.1) | – | ||
| 12–24 | 92 (33.1) | – | 13 (59.1) | – | ||
| >24 | 6 (2.2) | – | 0 (0.0) | – | ||
| Unknown | 18 (6.5) | – | 0 (0.0) | – | ||
| Type of phototherapy‡ | ||||||
| Bilirubin blanket | 173 (62) | – | 9 (40.9) | – | 0.049* | |
| Single phototherapy | 76 (27.3) | – | 7 (31.8) | – | 0.651 | |
| Double phototherapy | 71 (25.5) | – | 6 (27.3) | – | 0.858 | |
| Triple phototherapy | 34 (12.2) | – | 3 (13.6) | – | 0.742 | |
| Exchange transfusion | 0 (0.0) | – | 0 (0.0) | – | 1.000 | |
| Other | 0 (0.0) | – | 0 (0.0) | – | 1.000 | |
| Unknown | 26 (9.4) | – | 5 (22.7) | – | 0.062 | |
‡, the count for triple, double and single phototherapy may include bilirubin blanket based on patient chart documentation; *, P<0.05. N, number; %, percentage; SD, standard deviation; hrs, hours.
Risk factors for re-admission to hospital
Table 3 outlines components in the management of infants with hyperbilirubinemia that were determined a priori as relevant to our outcome of interest. Infants who did not re-present were discharged with a mean (SD) bilirubin level of 102.43 (39.46) µmol/L below threshold and the infants who were re-admitted were discharged with mean (SD) bilirubin of 87.92 (35.37) µmol/L below threshold (P=0.111). Interestingly, mean bilirubin levels on repeat presentation were lower than for those who did not re-present and who had initially been admitted (P=0.037).
In both groups, infants were discharged with mean bilirubin levels well below targeted treatment thresholds and outside of the 50 µmol/L margin. No other factors were statistically significant.
Table 4 summarizes the bivariate analysis of patient factors and bilirubin details in our study population. Significant differences in the mean bilirubin level at which phototherapy was initiated and department of discharge were found between non-exclusively breastfed infant who were re-admitted and who were not re-admitted. To better understand these findings, we ran two separate logistic regression models. The first included variables significant at P<0.05 from the bivariate analysis. Table 5 shows only “other method of feeding” as significant (OR =0.13, 95% CI: 0.05–0.35, P<0.001). A second model was run to include any additional predictors that were significant at P<0.10 at the bivariate level (family history of jaundice). Again, only “other method of feeding” remained significant.
Table 4
| Patient variables | Re-admission following single course phototherapy | P value | |
|---|---|---|---|
| Yes (N=22) | No (N=278) | ||
| Bilirubin proximity to threshold at phototherapy initiation, median in µmol/L (IQR) | −4.7 (−21.1 to 31.9) | 4.8 (−21.3 to 24.8) | 0.959§ |
| Bilirubin level at start of phototherapy, mean rank in µmol/L | 112.91 | 152.95 | 0.037§* |
| Bilirubin proximity to threshold at time of discharge, median in µmol/L (IQR) | 84.65 (66.10–110.9) | 100.25 (78.8–124.25) | 0.097§ |
| Bilirubin within threshold for treatment at phototherapy initiation, N (%) | 7 (31.8) | 119 (42.8) | 0.676‡ |
| Bilirubin within but below threshold for treatment at time of discharge, N (%) | 4 (18.2) | 26 (9.4) | 0.255‡ |
| Breastfed by mouth only, N (%) | 11 (50.0) | 30 (10.8) | <0.001‡* |
| Other feeding methods, N (%) | 11 (50.0) | 248 (89.2) | <0.001‡* |
| Discharge ward | 0.032* | ||
| NICU | 2 (9.1) | 74 (26.6) | |
| Paeds | 7 (31.8.8) | 112 (40.3) | |
| MBCU | 13 (59.1) | 91 (32.7) | |
| Evidence of rebound, N (%) | 1 (4.5) | 12 (4.3) | 1.000 |
| Phototherapy duration, median in hours (IQR) | 19.25 (14.25–29.25) | 20.25 (14.00–27.00) | 0.847§ |
| Phototherapy type, N (%) | 0.111‡ | ||
| Bilirubin blanket only | 2 (9.1) | 62 (22.3) | |
| Single phototherapy | 5 (22.7) | 45 (16.2) | |
| Multiple modes of therapy | 10 (45.5) | 145 (52.2) | |
| Unknown | 5 (22.7) | 26 (9.4) | |
| Gestational age in weeks, N (%) | 0.199 | ||
| <38 | 12 (54.5) | 121 (43.5) | |
| 38 | 8 (36.4) | 147 (52.9) | |
| Age at presentation, median in days of life (IQR) | 2 (1–3) | 3 (2–4) | 0.335 |
| Risk Stratification, N (%) | 0.199 | ||
| Low | 8 (36.4) | 147 (52.9) | |
| Medium | 12 (54.5) | 121 (43.5) | |
‡, calculated by Fisher’s exact test; §, calculated by Mann-Whitney U; *, P<0.05. N, number; MBCU, mother baby care unit; NICU, neonatal intensive care unit; IQR, interquartile range; %, percentage.
Table 5
| Variable | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Bilirubin level at start of phototherapy | 0.99 | 0.98–1.00 | 0.14 |
| Other method of feeding | 0.13 | 0.05–0.35 | <0.001* |
| Department of discharge (MBCU) | 1.39 | 0.36–5.38 | 0.63 |
| Department of discharge (NICU) | 0.33 | 0.05–2.22 | 0.25 |
*, P<0.05. MBCU, mother baby care unit; NICU, neonatal intensive care unit; IQR, interquartile range; %, percentage; CI, confidence interval.
The 22 re-admitted infants were also compared to the 14 who re-presented but did not require re-admission. No significant difference was shown when comparing initial length of stay, etiology of hyperbilirubinemia, phototherapy method and duration, age at admission, age when phototherapy was initiated, discharge and gestation. No significant difference was noted when similar analysis was performed between re-admitted infant and those with single course phototherapy who did not re-present to hospital (not shown).
Discussion
Current Canadian guidelines clearly outline the importance of prevention, detection, and management of infants with unconjugated hyperbilirubinemia (1). Although nomograms supporting recommendations for re-evaluation of serum bilirubin based on infant risk (1) and initiation of intensive phototherapy has been widely distributed (4), management following initiation of phototherapy has not been as clearly outlined. This results in an opportunity for further recommendations and practice standardization.
Our results reveal important variations to highlight despite lack of statistical significance in the frequency of bilirubin level checks, as well as in the documentation of choice and duration of phototherapy.
We found that infants bilirubin levels were checked 2–3 times a day while admitted. Though there does not appear to be any statistically significant differences among the groups, there could be the clinical impact to the patient and family of repeated unnecessary bilirubin checks (i.e., pain for the infant, distress to families, etc.). In general, infants were discharged with mean bilirubin levels well below the phototherapy threshold. However, no bilirubin level was checked post-discontinuation of therapy in 17% of infants. It was unclear whether a post-discontinuation level was done for 4 infants who were re-admitted which could impact the statistical significance of a post-discontinuation level with risk of re-admission. Therefore, the risk of re-admission for infants without a bilirubin check post-discontinuation of therapy could be much higher, making the safety of such a practice questionable. From these observations, further studies would be needed to support the proposition of establishing 2 standard bilirubin checks: 12 hours after phototherapy initiation and 12 hours post-discontinuation to ensure no rebound while maintaining safety and limiting testing.
We found 3 important factors in our aim to identify predictors of infant re-admission for second course of phototherapy. These were bilirubin level at start of phototherapy, ward of discharge and method of feeding (e.g., breastfed by mouth only vs. other feeding methods).
Our data suggest the threshold to treat hyperbilirubinemia on second presentation is lower than at initial presentation with mean (SD) bilirubin values for those re-admitted, of 232.19 (67.18) and 265.72 (69.60) µmol/L, respectively (P=0.037). A 2012 national review of repeat visits to pediatric EDs in the United States identified that children less than 1 year of age who had been recently discharged were more likely to be re-admitted to hospital (17). In that review it was postulated that due to their medically fragile nature, their inability to communicate illness, and the higher parental concern at this age, physicians may be biased towards conservatively re-admitting an infant who has a repeat hospital visit. As it pertains to hyperbilirubinemia, providers may feel that the relatively non-invasive nature of a short course of phototherapy may be of benefit in assuaging parental concerns and offering an opportunity for further evaluation when infants re-present with mild-to-moderate hyperbilirubinemia. Furthermore, providers may question the initial reason for hyperbilirubinemia and prefer an in-hospital observation period rather than repeated ED visits, considering the widespread perception that patients with repeat visits are thought to be a “sicker population” (18). Further investigation is needed to determine physician perception of re-presentation and the reasons for the significant difference in bilirubin level at the start of phototherapy between the two groups.
There was a significant difference in infants re-admitted depending on department of discharge. Few patients were re-admitted from the neonatal intensive care unit (NICU) where more detailed documentation was noted, compared to a third of patients coming from the pediatric clinical teaching unit (CTU) and over half of patients from the mother baby care unit (MBCU). One potential explanation could be that infants in the NICU often have multiple issues prolonging their stay, resulting in longer observation periods post-discontinuation of phototherapy. It could also explain the frequent bilirubin level re-assessments and clearer detail in phototherapy documentation. Similarly, more patients may have been re-admitted following discharge from the MBCU because of shorter lengths of stay in that department. The variation in documentation and potential contribution to re-presentation suggests the need for one standard phototherapy record template for all providers.
Our results demonstrate the overwhelming prevalence of breastfeeding failure as the most common etiology of hyperbilirubinemia that is also reflected in other studies (11-14). In our logistic regression models, exclusive breastfeeding was the only identified factor that significantly predicted re-presentation to hospital. With this observation, it is not surprising that infants supplementing with formula were less likely to require re-admission. Based on the data collected, we are unable to determine what factors may have contributed to this particular population being re-admitted (e.g., whether breastfed infants were more dehydrated at second presentation compared to initial discharge, what their intake volumes were in between discharge and re-presentation, etc.). Despite this, it may suggest that supplementation should be encouraged for infants admitted for phototherapy. Further studies addressing this observation need to be considered before this would become a discharge recommendation.
We identified three key limitations with our study. First, the number of infants who re-presented to hospital may be underestimated as this chart review only had access to records of infants included in the catchment area of LHSC, using a specific electronic medical record (EMR). As a result, infants who presented to other community hospitals with different EMRs were not captured. Second, documentation regarding the application, type, and discontinuation of phototherapy was variable depending on the department admitting the patient. Using physicians’ orders to determine timing of therapy may have had one of two effects. On one hand, this may have underestimated the duration of therapy in the case of discontinuation of therapy due to potential delays between order placement and execution. On the other, it could have overestimated the duration of treatment in the case of therapy initiation. Third, during the chart review, it became clear that there was ambiguity to the term “phototherapy”. On some wards it was used to mean bilirubin blanket, while on others it was used for single or double overhead lights. The differences in documentation of these factors may have underestimated their association to re-presentation.
Another factor of interest influencing bilirubin level interpretation was the initiation of transcutaneous bilirubin checks on delivery wards vs. capillary bilirubin samples. Although transcutaneous bilirubin has been shown to correlate well with serum bilirubin, in some patient populations it is an overestimate (19). LHSC began using transcutaneous bilirubin in October 2014 in only select areas of the hospital. It is unclear whether this may have impacted bilirubin interpretation with respect to phototherapy threshold and treatment initiation.
In summary, to our knowledge this is the first study looking at predictors of re-admission for infants with jaundice after an initial course of phototherapy. Other than exclusive breastfeeding, our findings did not identify other predictive factors for infant re-presentation and re-admission to hospital for repeat phototherapy. Interestingly, the threshold to treat a high bilirubin level appears to be lower on repeat presentation. With regard to practice variations, although there does appear to be some difference in the number of bilirubin checks during admission, they do not appear to have any consequence to re-presentation to hospital. This reflects an important take home message: current discharge criteria and target bilirubin cut-offs in the care of patients with hyperbilirubinemia requiring phototherapy is not standardized and may contribute to the challenge of identifying modifiable risk factors for re-presentation. Further studies should aim to standardize hyperbilirubinemia management, demonstrating optimal timing for serum bilirubin level measurements. This would contribute to determining specific bilirubin cut-off values that would avoid re-presentation without prolonging length of initial stay. Furthermore, a trial of standardized phototherapy documentation records, as well as qualitative research exploring healthcare providers’ comfort level with management of infants who re-present for unconjugated hyperbilirubinemia may be of future value.
Acknowledgments
Funding: All phases of this study were supported by a grant from the Department of Paediatrics Resident Research Grants Program, at Western University.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://pm.amegroups.com/article/view/10.21037/pm-21-89/rc
Data Sharing Statement: Available at https://pm.amegroups.com/article/view/10.21037/pm-21-89/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://pm.amegroups.com/article/view/10.21037/pm-21-89/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Western University research ethics board of London Ontario (REB#107955) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Barrington K, Sankaran K. Guidelines for detection, management and prevention of hyperbilirubinemia in term and late preterm newborn infants. Paediatr Child Health 2007;12:1B-12B. [Crossref]
- Sgro M, Campbell D, Shah V. Incidence and causes of severe neonatal hyperbilirubinemia in Canada. CMAJ 2006;175:587-90. [Crossref] [PubMed]
- van Imhoff DE, Dijk PH, Hulzebos CV. Uniform treatment thresholds for hyperbilirubinemia in preterm infants: Background and synopsis of a national guideline. Early Hum Dev 2011;87:521-5. [Crossref] [PubMed]
- American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2004;114:297-316. [Crossref] [PubMed]
- Romagnoli C, Tiberi E, Barone G, et al. Validation of transcutaneous bilirubin nomogram in identifying neonates not at risk of hyperbilirubinaemia: A prospective, observational, multicenter study. Early Hum Dev 2012;88:51-5. [Crossref] [PubMed]
- Bromiker R, Bin-Nun A, Schimmel MS, et al. Neonatal Hyperbilirubinemia in the Low-Intermediate-Risk Category on the Bilirubin Nomogram. Pediatrics 2012;130:e470-5. [Crossref] [PubMed]
- Yu ZB, Han SP, Chen C. Bilirubin nomograms for identification of neonatal hyperbilirubinemia in healthy term and late-preterm infants: a systematic review and meta-analysis. World J Pediatr 2014;10:211-8. [Crossref] [PubMed]
- Bhutani VK, Stark AR, Lazzeroni LC, et al. Predischarge Screening for Severe Neonatal Hyperbilirubinemia Identifies Infants Who Need Phototherapy. J Pediatr 2013;162:477-82.e1. [Crossref] [PubMed]
- Kaur S, Chawla D, Pathak U, et al. Predischarge non-invasive risk assessment for prediction of significant hyperbilirubinemia in term and late preterm neonates. J Perinatol 2012;32:716-21. [Crossref] [PubMed]
- Chawla D, Jain S, Dhir S, et al. Risk Assessment Strategy for Prediction of Pathological Hyperbilirubinemia in Neonates. Indian J Pediatr 2012;79:198-201. [Crossref] [PubMed]
- Chang PF, Lin YC, Liu K, et al. Risk of Hyperbilirubinemia in Breast-Fed Infants. J Pediatr 2011;159:561-5. [Crossref] [PubMed]
- Chen YJ, Chen WC, Chen CM. Risk factors for hyperbilirubinemia in breastfed term neonates. Eur J Pediatr 2012;171:167-71. [Crossref] [PubMed]
- Huang HC, Yang HI, Chang YH, et al. Model to Predict Hyperbilirubinemia in Healthy Term and Near-Term Newborns with Exclusive Breast Feeding. Pediatr Neonatol 2012;53:354-8. [Crossref] [PubMed]
- Chang PF, Lin YC, Liu K, et al. Identifying term breast-fed infants at risk of significant hyperbilirubinemia. Pediatr Res 2013;74:408-12. [Crossref] [PubMed]
- Healthcare Insurance Reciprocal of Canada Web site. Risk Reference Sheet: Failure to Identify/Manage Hyperbilirubinemia. In Acute Care (Maternal/Newborn). March. 2016 [cited 2016 Jun 5]. Available online: https://www.hiroc.com/resources/risk-reference-sheets/failure-identifymanage-hyperbilirubinemia
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-81. [Crossref] [PubMed]
- Cho CS, Shapiro DJ, Cabana MD, et al. A National Depiction of Children With Return Visits to the Emergency Department Within 72 Hours, 2001–2007. Pediatr Emerg Care 2012;28:606-10. [Crossref] [PubMed]
- Alessandrini EA, Lavelle JM, Grenfell SM, et al. Return Visits to a Pediatric Emergency Department. Pediatr Emerg Care 2004;20:166-71. [Crossref] [PubMed]
- Olusanya BO, Imosemi DO, Emokpae AA. Differences Between Transcutaneous and Serum Bilirubin Measurements in Black African Neonates. Pediatrics 2016;138:e20160907. [Crossref] [PubMed]
Cite this article as: Bravo G, Miller MR, Zizzo AN. Factors associated to hospital re-admission of infants previously treated for hyperbilirubinemia. Pediatr Med 2022;5:4.