
Understanding adolescent anxiety disorders through the lens of decision science: towards a mathematical psychiatry
Introduction
This is an introduction to Anxiety Disorders in adolescents through the lens of cognitive science, in particular that part of cognitive science that deals with human decision making. The goal is to recognize that psychopathology is properly understood as an extension of ordinary behavior, rather than a distinct state of mind that differs fundamentally from a ‘healthy’ state of mind. Decision making, and in particular differences in how people make decisions, may be the best lens through which to examine the emotions and behaviors involved in anxiety disorders. This conceptualization is not only theoretically sound, but also may reduce stigmatization of Anxiety Disorders by revealing the fundamental continuity between ordinary and ‘anxious’ behavior (1). The conceptualization introduced here relies on two key paradigms, both related to decision making: Rational Choice Theory (RCT) and Fear Learning. RCT, borrowed from classical microeconomics, states that, given a set of preferences and beliefs about how the world works, individuals act so as to maximize their own subjective benefit, or utility. Fear Learning is a type of behavioral conditioning in which a person learns to fear a stimulus after it becomes associated with a negative outcome. Both paradigms explain aspects of ordinary decision making, and both can be subject to anomalies that result in anxious emotions and behavior.
Critics of RCT have pointed to various well-documented cognitive slips and biases that suggest that humans are not perfectly rational and that RCT therefore cannot be an accurate account of human decision making (2). The argument maintains that the rational “Homo economicus” postulated by traditional RCT simply isn’t an accurate picture of real humans and their behavior. The best response to this argument was made by Richard Thaler, Nobel Laureate for his work in behavioral economics, who made the following point. Let us agree that both these statements are false: (I) RCT is completely true, and (II) RCT has nothing to teach us about human behavior (3). His point was that while RCT is not a perfect model of human decision making, it nevertheless is an important starting point to analyze decisions. If we want to understand human decisions, we should start by examining how a perfectly rational agent would behave, and then look for the normal human deviations from that position. By some accounts that is what the program of Behavioral Economics is all about—start with an assumption of rationality and then study all the ways humans do and do not behave according to the assumption. This discussion will follow that model and builds on RCT as modified by the insights and empirical findings of behavioral economics.
This conceptualization of Anxiety Disorders also draws on the “Dual System” model of the brain, as elaborated in the best-selling book by Daniel Kahneman, Thinking, Fast and Slow (4). That model proposes that we have two information-processing systems, each with a unique processing style and that are activated in distinct situations. System Two—the system most people think of when they think of ‘normal’ information processing—is methodical, logical, and comparatively slow. It helps us solve math problems, focus on a difficult book, or navigate a busy intersection. System One, on the other hand, is instinctive, emotional, and faster. It relies on what people call gut instinct. It makes extensive use of heuristics (quick rules of thumb) and cognitive biases in order to accelerate processing in familiar or predictable contexts. In this discussion ‘bias’ does not mean a negative attitude toward others, but rather a preconfigured belief or internal algorithm that we rely on instinctively when a situation calls for it. Such biases may be useful or not, depending on the situation. System One is very effective for reading and responding to STOP signs, staying safe from fire, or driving home from work on a routine route, but it fares poorly if applied to learning calculus, for example. As we will see, although there is no perfect correlation, System Two is associated with RCT, and anomalies in System Two result in anxious worry. System One is associated with Fear Learning, which is the root of anxious avoidance, the powerful drive to avoid places, persons, or things that have become sources of unfounded fear (5).
Prevalence and presentations of Anxiety Disorders1
Anxiety Disorders present in multiple forms, and DSM-5 made significant changes from previous DSM editions to the criteria and classification of these disorders. Six disorders are included in the updated chapter on Anxiety Disorders (estimated incidence rate among U.S. adolescents in parentheses): Specific Phobia (19.3%), Social Anxiety Disorder (9.1%), Separation Anxiety Disorder (7.6%), Agoraphobia (2.4%), Panic Disorder (2.3%), and Generalized Anxiety Disorder (2.2%) (6). Obsessive-Compulsive Disorder and Posttraumatic Stress Disorder, previously included amongst the Anxiety Disorders, were each removed and given their own sections in DSM-5. Anxiety Disorders as a class have an adolescent incidence rate of 31.9%, making them the most common class of mental disorders among adolescents. Adolescent females are diagnosed with Anxiety Disorders at higher rates than adolescent males (38.0% vs. 26.1%) (6).
One way of organizing Anxiety Disorders is to look at them through the lens of the type of stimuli that provoke an anxious response. At one extreme, Specific Phobias occur when a single stimulus (or closely related class of stimuli) provokes intense, excessive fear. As the name suggests, these phobias are very particular, and therefore may only be triggered by specific objects or settings. At the other extreme, patients with Generalized Anxiety Disorder experience pervasive and enduring anxiety about a whole range of topics, from the expiration date on the milk carton to the risk of nuclear conflagration. As a result, symptoms of Generalized Anxiety Disorder will be present in many different settings and may be present without any triggering at all. The other specified Anxiety Disorders fall between these poles, each with its own class of trigger stimuli: Social Anxiety Disorder (fear of judgment and embarrassment in social settings), Separation Anxiety Disorder (fear when not in close physical presence of a parent or caretaker), Agoraphobia (fear of being unable to escape public spaces or find help), and Panic Disorder (both the occurrence of, and fear of recurring, panic attacks). Of course, not all presentations of anxiety will fit precisely into one of these diagnoses, even when such anxiety may be severe, impairing, and obviously pathological. Anxiety of this form may be diagnosed as “Anxiety Disorder – Not Otherwise Specified (NOS),” a catch-all diagnosis which reflects our humility in the face of the heterogeneity of anxious presentations.
Despite the heterogeneity of anxious presentations, two symptoms recur across the majority of presentations: worry and avoidance (7-9). These are the hallmarks of an anxious person. Worrying is a central cognitive experience for a person with anxiety. Whether it’s worrying about immediate risks or future catastrophes, specific situations or life in general, anxious people have frequent thoughts about what might go wrong. This cognitive symptom is often accompanied by emotional discomfort and by physical concomitants such as sweating, a racing pulse, aching or tired muscles, and a dry mouth (10). Worrying is related in complex ways to avoidance, the behavioral complement to cognitive worry. Beset on all sides by perceived risks, an anxious person will hunker down and avoid entering any situation that could trigger the feared outcomes. Not only physical settings but also sensory experiences, people, abstract concepts, and even memories may become subject to anxious avoidance in this way. The idea of people avoiding places is easy to relate to, but people avoiding their own thoughts may seem unusual. Actually, it is common for people to say, in regard to some negative thought, “I don’t want to even think about that.” But avoiding thoughts in your own head is often difficult, and it can be dangerous when that thought is needed for future planning or achieving safety in a dangerous situation. This raises the question as to how RCT and Fear Learning become distorted in an anxious person to cause worry and avoidance.
RCT and anxious worry
RCT holds that people act with the goal of increasing their own satisfaction, or what economists call subjective utility (11). Note that the word ‘subjective’ here merely refers to an individual’s personal sense of what they consider valuable. So, the subjective utility of chocolate ice cream is different for individuals who love, hate or are indifferent to this dessert. Two key inputs determine what will or won’t increase subjective utility for a particular individual: preferences and probabilities. Preferences refer to the benefit (utility) or penalty (disutility) that are the outcomes of our choices, and probability refers to the likelihood of a possible outcome actually happening. Say I am deciding whether to bring an umbrella to work. If I leave it home, I run the risk of being drenched, which I ascribe a subjective disutility of –10, but I may also enjoy the clear day without needlessly carrying an umbrella, for a subjective utility of +5. Note that when we assign numbers to these utilities, they are relative numbers (like points in a game) for comparing positive or negative experiences to each other, but these don’t represent absolute unit values. There are ways to assign actual dollar values to these utilities, but this complexity is not needed for our discussion. Returning to our choice, if I bring the umbrella and it rains, I will only suffer a little (subjective utility =–4); if it doesn’t rain, I enjoy the clear day but still bear the cost of carrying the umbrella (subjective utility =+3). First note that I choose whether or not to take the umbrella, but the weather determines which actual outcome I experience. Fortunately, I may have some information about the weather, and thus about the likelihood of different outcomes for each of my umbrella choices. Suppose I believe there is a 75% chance of rain. My options are represented in Figure 1.
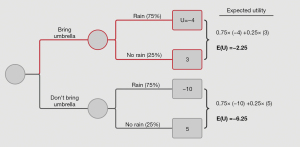
If I bring an umbrella, there is a 75% chance it rains and I get utility of ‒4 and a 25% chance it doesn’t rain and I get a utility of 3. Combining both weather scenarios (rain or no rain), my total Expected Utility for bringing an umbrella equals . My total Expected Utility for not bringing an umbrella equals (Table 1). According to RCT, if I believe there is a 75% chance of rain, I will choose to bring an umbrella because that choice has the greatest expected utility. Note that when there is a 75% chance of rain my choices involve minimizing negative utility; for today, positive utility is not on the menu.
Table 1
| [1] | Bring umbrella & rain | =75% × (‒4) | =‒3 |
| [2] | Bring umbrella & no rain | =25% × (3) | =0.75 |
| [3] | Don’t bring umbrella & rain | =75% × (‒10) | =‒7.5 |
| [4] | Don’t bring umbrella & no rain | =25% × (5) | =1.25 |
Each row reflects a separate possible outcome with the associated calculation of expected utility.
As described above, RCT is an obvious example of System Two processing. In order to reach the conclusion that I should bring an umbrella, I had to follow a sequence of steps that required dedicated focus and analysis. First, I had to inspect my own preferences to determine the relative costs and benefits, for me, of getting wet with and without an umbrella, as well as for carrying around an umbrella. I had to generate a value for the probability of rain, either by gathering data or making a guess. I had to calculate the Expected Utility value of each branch of the decision tree, and finally I had to compare these Expected Utilities to determine which choice to make. This kind of deliberate, methodological approach to problem solving is precisely where System Two excels. If this seems like an unrealistic model of decision making, why do people regularly seek information on the probability of rain when making this decision?
RCT explains the variability of human behavior by reference to the two inputs to the model, preferences and probabilities. You may choose not to bring an umbrella, either because you are less averse to getting drenched than I am (i.e., your utility for “don’t bring umbrella & rain” is less negative than mine), or because you have a different belief about the probability of rain. Either way, the balance of Expected Utilities for each outcome determines which decision you and I make. Neither choice is better or more “rational”; we both make a rational choice given our preferences and probability beliefs.
According to RCT, anxious individuals make choices just as their non-anxious peers do, by assigning utilities and probabilities and then making the choice which maximizes Expected Utility. Anxious individuals, however, are distinguished merely by the specifics of their beliefs about the utilities and probabilities of outcomes, which diverge significantly from the beliefs of non-anxious individuals (12). Indeed, while “deficits” and “biases” in the decision-making of anxious individuals have been extensively documented (13,14), these findings focus primarily on heightened risk sensitivity, which may be interpreted as changes to the ‘inputs’ of RCT, and impaired learning due to anxious avoidance, which we address in the following section on Fear Learning.
Variation of the RCT inputs explains ordinary behavioral variability, and extreme input values explain the emergence of anxious worry. There are two ways an anxious person may stand out—abnormal utilities and abnormal probabilities—and these correspond to distinct clinical presentations of anxious worrying. First, abnormal utility values work as follows.
Say one must decide how many hours to study for an upcoming test. Aaron and Gillian have different utilities for passing the test but neither has an Anxiety Disorder. Their choices are represented in Figures 2,3.
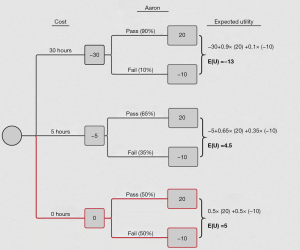
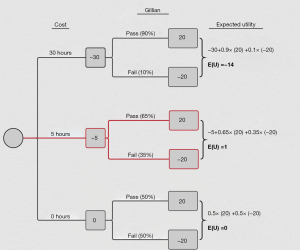
Aaron and Gillian have the same probability expectations that a certain number of hours of study will lead to a certain probability of passing. Both think that 30 hours of study will give them a 90% chance at passing, 5 hours will give them a 65% chance, and no study will still give them a 50% chance. Both consider each hour of study a loss of enjoyment and rate it as ‒1 utility. The difference between them is that for Gillian failing the test is really bad (utility =‒20), whereas Aaron values it only ‒10. The question is, how would each of these different rational agents choose the right amount of study time? Following the calculations in their respective decision trees, Gillian maximizes her Expected Utility by studying for five hours and Aaron maximizes his by not studying at all. Again, both make a perfectly “rational” choice given the preferences and beliefs that inform their decision trees.
Now consider Max, who also must make a choice but has an Anxiety Disorder. In his case, we expect to find ‘abnormal’ utility values that lie outside the ordinary variability observed between Aaron and Gillian. Max will exhibit the RCT-equivalent of what a clinician might label “catastrophizing.” Max is so scared of failing he sees it as an overwhelmingly negative outcome that will significantly harm his college career. We might capture this by saying that Max values failing the test at ‒400, twenty times worse than his peer Gillian. Max’s decision tree is depicted in Figure 4.
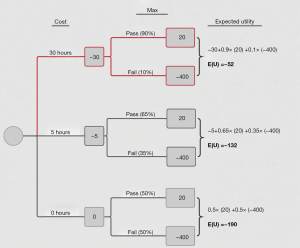
As the decision tree illustrates, Max will choose to study for 30 hours under these assumptions—and then still, he expects a much worse outcome (utility =‒52) than either Aaron (utility =+5) or Gillian (utility =+1) does. Note that Max’s parameters are identical except for the utility of failing the test. That is, Max does not enjoy studying more than his peers (the utility of studying is ‒1 per hour across individuals), he is not worse at studying (the marginal probability of passing for each hour of additional studying is the same for each individual), and he does not get more utility from passing than his peers (each has a utility of +20). Max differs from Aaron and Gillian only in that he believes that failing the test will be a much worse—it will be a catastrophe.
Another example is Jim, who is like Max but instead of an extreme disutility he assigns an extremely high probability to failing the test. Numerically, Jim and Max face decision trees with similar outcomes, because Expected Utility is simply the product of the utility and probability. For example, Jim may value failing the test at ‘just’ ‒40, but he starts off with a much lower expectation for the probability of passing, say 10%. As a result, his starting point before any studying yields a much lower Expected Utility (‒34) than Aaron or Gillian’s starting beliefs do. Moreover, even if Jim’s confidence (probability of passing) increases at the same rate as his peers’, for any given number of hours studied he will always be more pessimistic about passing than the rest. His utility-maximizing choice—studying 5 hours—still results in a significantly negative subjective utility (‒30) (Figure 5).
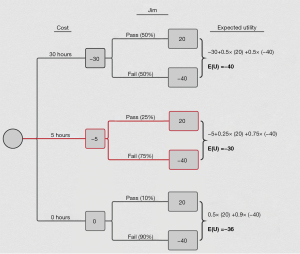
Though structurally similar, Jim’s clinical presentation will be quite different from Max’s. Rather than worrying about the catastrophic consequences of not studying enough, Jim instead fixates on the near inevitability, as he perceives it, of failing the test, regardless of his effort. He is worried and hopeless. Even at the utility-maximizing point, Jim still only believes he has a 25% chance of passing the test. While seeming like abstract exercises, the theoretical types which Max and Jim represent actually correspond closely to clinical presentations of Anxiety Disorders, lending support to this approach.
Abnormal utilities and probabilities cause anxious worry because they turn every decision into a potential catastrophe. Aaron and Gillian differ in the disutility they would get from failing the test—but neither approaches the terrible consequences that Max and Jim anticipate. Though colloquially we might say that Gillian “worries” about the test relative to Aaron, it is not the type of paralyzing, all-consuming worry that sends one to a therapist. Moreover, Gillian can assuage her worry by studying for five hours. Max on the other hand doesn’t realistically have the same option. Given his beliefs, Max’s optimal choice would be to study for 30+ hours; any less than that and he will worry about being inadequately prepared for the test. However, Max’s worry is not confined to this test, but instead pervades his life. He may escape one or two sources of anxiety by following the RCT-suggested path (study more), but he will not be able to do this for every situation. This also explains why a single source of anxiety can often motivate harder work, while multiple simultaneous sources of anxiety will paralyze the afflicted individual. Because Max cannot make the optimal choice in every setting, he will constantly feel inadequately prepared for possible negative outcomes, each of which causes him more and more worry.
Whether it is by catastrophizing (extreme negative utilities) or fatalism (high probabilities for bad outcomes), Max and Jim face a decision tree that looks very different from that facing their non-anxious peers. To them ordinary decisions do not look like “ordinary decisions” but rather like a series of catastrophes waiting to happen. Beset by such decisions on all sides, the anxious person may become paralyzed with worry.
Fear learning and anxious avoidance
Fear learning is a form of associative learning by which an organism learns to fear stimuli that are not intrinsically aversive. Fear learning is a form of conditioning. In conditioning, researchers start with a stimulus (the “Unconditioned Stimulus”, or US) that is known to provoke some response (the “Unconditioned Response”). During the conditioning phase, a neutral stimulus is repeatedly presented together with the US, until the subject begins to associate the neutral stimulus with the unconditioned response. At this point the US is removed and the neutral stimulus, now called the “Conditioned Stimulus” (CS), evokes the same response as the unconditioned response on its own (and this is now called the “Conditioned Response”) (15). Through this process neutral stimuli of all sorts can acquire the power to provoke an automatic response in an individual. This automatic response may in turn arouse a pattern of feelings and/or thoughts, which also become associated with the conditioned stimulus, thus lending the conditioned stimulus an emotional quality and motivational efficacy in the individual’s experience.
In fear learning, classical conditioning operates on an aversive experience to generate fear of a stimulus. A seminal study—the “Little Albert” experiment (16)—can help illustrate the process. The goal of the study was to examine the possibility of creating a “fear” out of a non-threatening situation. The experiment used a white lab rat as the stimulus. Before the experiment started, Albert showed no fear of the rat at all. Then the experimental conditioning began. Each time the rat was presented, the researchers would blast an unpleasant noise that scared Albert. Eventually, the researchers presented the rat to Albert without the accompanying sound. As predicted, Albert was terrified, showing involuntary fear responses and attempting to move away from the rat.
Albert was conditioned in an experimental setting where researchers controlled the conditions of every subject-stimulus interaction, with the explicit intention of creating a conditioned fear. Fear learning is not confined to the laboratory, though. In real life, we constantly encounter situations that engender the conditions for fear learning. Any time a stimulus provokes a response, whatever was paired with that stimulus may become a conditioned stimulus that will evoke the same response on its own in the future. Say a teacher notices one student struggling and intervenes by asking her to write her homework answers on the board every day for a week. She hates math, so being called on like this provokes intense fear. The next time she has that class, she immediately begins to worry and exhibit the same reactions as before, even if the teacher doesn’t actually call on her this time. It doesn’t matter that the actual fearful stimulus (the US) is not present. Through repeated pairings with the US, the class itself has now become a conditioned stimulus that on its own provokes the fear response.
Like other forms of conditioning, fear learning can also be subject to ‘generalization,’ which occurs when the boundaries that define the conditioned stimulus are expanded (17). Take our student from above. She was conditioned to exhibit stress whenever she has math class. But what if she is asked to do the same in English class? If she exhibits the conditioned response in this setting, we say that “generalization” has occurred. The original conditioned stimulus—being called on in Math class—has been generalized to include all classes. The student thus begins to exhibit the conditioned response in more and more settings, which could eventually lead to school refusal or delinquency. (The opposite of generalization, ‘discrimination,’ may also be relevant and is addressed below.)
The fear learning paradigm suggests two ways in which individuals with anxiety disorders may differ from their non-anxious counterparts, both of which have been empirically confirmed (18). First, individuals with anxiety might have a lower threshold for the initial establishment of a conditioned fear. For an ‘ordinary’ student, it might take a month of being called on before he begins to exhibit a conditioned response, whereas the student in our example needed only a week before the conditioning was established. Indeed, research has begun to examine the rate of fear learning (and “extinction,” or forgetting) in humans and mice (19-21), finding that differences in this rate correlate with the intensity of anxious symptoms (22,23). As a result of a greater fear learning rate, anxious individuals not only develop a conditioned fear response sooner than non-anxious individuals for a given stimulus, but they also do so in response to a greater number of scenarios. This may explain how a Specific Phobia can attach to seemingly innocuous or rare stimuli.
Anxious individuals also stand out by the way in which they engage in generalization (24). Some degree of generalization is expected and adaptive. Without it, one would have to experience every possible danger before developing adaptive, automatic responses. As expected, healthy individuals exhibit a range of generalization rates which correspond to distinct phenotypes of ‘ordinary’ fear generalization (25). But generalization can also run astray, creating fearful conditioned stimuli wherever the eye turns. Considering individuals with Anxiety Disorders, higher rates of generalization (compared to healthy controls) have been observed in patients with Generalized Anxiety Disorder (26), Panic Disorder (27), Posttraumatic Stress Disorder (28), and adolescents with any kind of Anxiety Disorder (29). Moreover, both anxious adolescents and adults exhibit greater generalization compared to non-anxious individuals (29,30). Heightened generalization contributes to a proliferation of perceived threats for the subject, creating the conditions for pervasive anxiety.
When fear learning runs amok—either through a lowered conditioning threshold or through a heightened generalization tendency—avoidance becomes the dominant behavioral response (31). Wherever they turn, anxious individuals find themselves surrounded by conditioned stimuli that provoke an automatic fear response, and as a result they feel constantly on edge. Because the individual’s response is conditioned—i.e., an automatic response to a learned stimulus—no amount of reasoning or evidence will mitigate the effect of the conditioned stimuli. Left without the ability to change the response on their own, the anxious person responds by avoiding the stimuli all together. And since the anxious person encounters conditioned stimuli wherever they turn, avoidance can evolve from a situation-specific response into a general pattern of behavior.
Fear learning can be thought of as an instantiation of System One. In fear learning, the brain exhibits its ability to rapidly and automatically learn about new threats and develop an adaptive response. When our student walks into a math classroom, she immediately begins to sweat, shake, etc. This is not the result of a conscious inference based on her own observational data, but rather an automatic reaction over which she has no control. Indeed, she may herself be unaware of what provoked the reaction. Yet her brain’s fear circuitry has identified this particular class as a ‘threat’ and initiated an ‘adaptive’ response that preempts the slower System Two response, which might have mitigated some of the fear.
A clinical example of this concerned firefighters who were First Responders during 9/11. Some of them developed a fear and avoidance of elevators as a result of this exposure. They were clear that they did not believe that getting into an elevator would likely lead to any harm, but nevertheless they could not even go near an elevator. This mismatch of System One and System Two processing, and their own recognition of the irrationality of it, made them feel like they were going crazy. A first step in their treatment was, therefore, an explanation of Fear Learning and the fear system’s failure to communicate with the other parts of the brain that were sure that elevators were in fact safe.
Assessment and treatment of pediatric anxiety disorders
In this section, we outline how to assess the presence, nature and severity of anxiety disorders, and the range of treatment frameworks and therapeutic options that are available for adolescent anxiety disorders. In the following section, we point to possible updates of treatment modalities based on the decision-making conceptualization of anxiety elaborated throughout this chapter.
The first step towards assessing a presumed pediatric mental health disorder is to administer a general screening test. The Pediatric Symptom Checklist [PSC] (32), available in 35-item and 17-item versions, is a freely accessible option that is quick to complete (less than 5 minutes, typically), easy to score, and is available in many languages. The PSC has three subscales: Attention Disorders, Internalizing Disorders, and Externalizing Disorders. If a youth scores five or higher on the Internalizing subscale, they should be administered rating scales to check for the presence of disorders with internalizing presentations, such as anxiety disorders and depression. (If they score seven or higher on the Externalizing or Attention subscales additional rating scales should also be administered.)
Anxiety disorders in children and adolescents present in unique ways that differ from adult presentations of anxiety. Accordingly, it is important to use rating scales that are tailored to them such as the Screener for Child Anxiety Related Disorders [SCARED] (33), the Pediatric Anxiety Rating Scale [PARS] (34), or the Multidimensional Anxiety Scale for Children [MASC] (35). In contrast, the Hamilton Anxiety Rating Scale (36), the Beck Anxiety Inventory (37), and the Overall Anxiety Severity and Impairment Scale (38) have not been validated in pediatric samples and are not recommended. The General Anxiety Disorder 7-item Scale (39), frequently used in primary care settings due to its brevity, was not specifically developed for pediatric populations, but has been validated in that setting and is therefore also considered an acceptable option (40).
If the anxiety rating scale indicates the likely presence of an Anxiety Disorder, additional assessment is required. The key is to combine information from the rating scale with a thorough clinical interview that covers the nature and severity of symptoms, the extent of functional impairment, and recent stressors or changes in the individual’s environment. Severity of symptoms and functional impairment are often taken to be synonymous, but distinguishing them can greatly enhance treatment. Additionally, anxiety disorders exhibit a moderate-to-high degree of genetic heritability (41,42), so care providers should review the family’s medical history for the presence of any anxiety disorders or other psychiatric conditions. Care providers should also obtain the patient’s relevant medical history, including physical and psychological health, medications, and any recent changes in behavior. Significant life events may also either cause or exacerbate symptomatic behavior and need to be identified. While exploring such life events, the care provider should be cognizant of possible developmental trauma, abuse, or neglect, which could be contributing to the patient’s current situation. Though DSM-5 no longer groups Post-Traumatic Stress Disorder (PTSD) under Anxiety and Related Disorders (43), PTSD may still present with many anxious symptoms and, therefore, must be considered. Finally, the assessment should address any immediate medical and safety needs, including a suicide assessment and safety planning, if appropriate.
A number of physical and psychiatric conditions complicate the differential diagnosis of anxiety disorders. Relatively common physical conditions with overlapping symptoms include hyperthyroidism, caffeinism (including from carbonated beverages), migraine, asthma, lead intoxication and seizure disorder (44). Less commonly, anxiety-like symptoms may also be a result of hypoglycemia, pheochromocytoma, cardiac arrythmias, or CNS disorder (delirium or brain tumor). Pediatric Acute-onset Neuropsychiatric Disorders Associated with Streptococcal Infection (PANDAS) refers to a pattern observed in some children who appear to develop Obsessive-Compulsive Disorder and/or Tic Disorders such as Tourette’s Syndrome following Group A beta-hemolytic streptococcal infections (i.e., “strep throat” or “scarlet fever”). However, the validity of the PANDAS diagnosis remains contested (45); it is included in ICD-11 (World Health Organization, 2020) but not in DSM-5 (American Psychiatric Association, 2013).
Psychiatrically, anxiety disorders must be distinguished from other conditions that may mimic the restlessness, irritability, and social awkwardness of anxiety disorders. Attention Deficit Hyperactivity Disorder (ADHD), PTSD, and Type 1 Bipolar Disorder can cause anxiety-like restlessness, as can some Psychotic Disorders. The irritability of an Anxiety Disorder may also be mistaken for ADHD, PTSD, Bipolar Disorder and Depression. Anxious worrying about performance in school may be mistaken for the effects of a Learning Disorder or a result of the social skills deficit common in Autism Spectrum Disorder. Finally, anxiety may cause children to withdraw from social engagement, again mimicking behaviors common to autism and Psychotic Disorders.
Once a complete diagnosis is determined, treatment should advance in an incremental, multimodal approach. A comprehensive treatment plan will consist of psychoeducation (for both the parent(s)/caretaker(s) and the child), consultations with school personnel or other significant adult caretakers, psychotherapy (starting with Cognitive Behavioral Therapy (CBT) but including other modalities, as appropriate), pharmacotherapy, and referral to a childhood mental health specialist, if required (46). For mild-to-moderate presentations, CBT is the first line treatment, as described below. For severe presentations, CBT should be augmented with medication from the outset.
CBT is the first line treatment for anxiety disorders. CBT is an empirically supported therapy model that explores the relationship between a person’s thoughts, feelings, and behaviors (47). The goal is to enable the patient to challenge and eventually change their own patterns of thought and behavior, thereby improving their quality of life. Unlike its psychoanalytic counterpart, CBT is a time-limited therapy, with a typical course of treatment lasting between twelve to sixteen sessions. Though many different adaptations and interpretations of the CBT model exist, most share a common set of components: psychoeducation, cognitive restructuring, somatic management skills and relapse prevention planning (48). As the most widely studied form of talk therapy, CBT has been broadly disseminated and many concepts have already begun to influence primary care, even in settings where specialized mental health care is not available.
Exposure-based CBT has the best empirical support for application in the context of pediatric anxiety disorders (46,49,50). Exposure-based CBT brings the patient in contact with an anxiety-inducing stimulus while preventing maladaptive responses. The exposure is typically gradual, often starting with an imaginary encounter (“Imagine yourself on stage in front of a room full of strangers…”) before progressing to in vivo exposure. During the therapy, the clinician also teaches the patient emotional self-regulation skills such as diaphragmatic breathing, visualization exercises, and techniques for challenging their own anxiety-prone thoughts. Together, the exposure and teaching are meant to desensitize the patient to the target stimulus while also equipping them with healthier coping skills and confidence for future challenges.
Psychotherapy may be supplemented by pharmacotherapy when talk therapy alone has not achieved the desired result. Medication may be particularly effective when the patient has a moderate-to-severe symptom pattern, when there is a comorbid psychiatric disorder, when the patient shows only partial or no response to therapy, or when they cannot even participate in therapy due to their baseline level of impairment (51). While studies have found that CBT and medication combined achieve better results than either treatment independently (46), in many cases CBT alone will achieve a satisfactory reduction of symptoms without incurring the side effects associated with medication. Thus, in mild-to-moderate cases CBT monotherapy remains the first line approach, and medication is added only for the reasons outlined above. Only when symptoms or functional impairment is severe is medication included in the first line treatment.
Two broad classes of medications have been associated with Anxiety Disorder treatment: antidepressants and anxiolytics. Within antidepressants, the serotonin-norepinephrine reuptake inhibitor (SNRI) duloxetine (brand name: Cymbalta) is the only FDA-approved treatment for Generalized Anxiety Disorder in children (52). There are currently no other FDA-approved treatments for pediatric anxiety disorders. The selective serotonin reuptake inhibitors (SSRIs) fluoxetine (brand name: Prozac), fluvoxamine (brand name: Luvox), and sertraline (brand name: Zoloft) are all FDA-approved for treating pediatric OCD (53), which, though no longer grouped under Anxiety and Related Disorders in DSM-5, shares many symptoms with DSM-5 anxiety disorders. Indeed, a range of SSRIs and SNRIs (duloxetine, venlafaxine, paroxetine, fluoxetine, fluvoxamine, sertraline) have proven safe and effective in randomized control trials for treating pediatric anxiety (54), However, these medications need to be administered with care and an awareness of the FDA boxed warning regarding suicidality (55). Regarding benzodiazepines, no randomized control trials have supported their use in pediatric settings. Moreover, the side effect profile, which includes disinhibition, cognitive impairment, and risk of seizures upon rapid discontinuation, is an additional reason to avoid usage. Finally, benzodiazepine use involves the risk of creating physiological or psychological dependence (56), especially in youths with substance use issues.
Updates to treatment informed by the decision-making model of anxiety
The efficacy of current treatments for anxiety disorders supports the decision-making model of anxiety presented here. CBT works precisely because it addresses the aberrant decision-making parameters that underlie an Anxiety Disorder, as explained above. The psychoeducation, cognitive restructuring and self-challenging aspects of CBT can work to change both catastrophizing (extreme negative utilities) or fatalism (high probabilities for bad outcomes). The exposure-focused CBT works to reverse fear learning through exposure and extinction.
Take Max for instance. Max is worried because he expects a horrible outcome if he fails the test, but he cannot possibly study enough hours to assuage his concern. In therapy, Max’s therapist will help him explore his beliefs about the test. What does he expect will happen if he fails? Why is this test different from others he has taken? If he does fail, what skills and resources can he rely on to cope? By challenging cognitive biases and highlighting objective indicators that enable him to relativize the feared outcome, CBT helps Max recognize that failing the test need not be the catastrophe he originally predicted (57).
The “exposure” of exposure-based CBT treatment directly targets the fear learning process that is responsible for anxious avoidance. When CBT therapists use exposure therapeutically it aligns closely with what classical conditioning theory calls “extinction.” More specifically, extinction is the gradual disappearance of a conditioned response after repeated exposures to the conditioned stimulus without the accompanying unconditioned stimulus (17). During exposure-based CBT, the patient will be repeatedly exposed to the conditioned stimulus without the aversive aspect that was expected and feared. Moreover, the therapist will encourage the patient to use cognitive and somatic relaxation techniques during the exposure to counter any automatic fear response generated by the nervous system. Through repeated experiences of the conditioned stimulus without negative consequences, the learned fear response becomes extinguished and the patient can re-establish a non-pathological relationship to the stimulus.
Decomposing anxiety into anxious worry and anxious avoidance suggests new avenues for treatment development. Moutoussis et al. (58) analyze the interaction of worry—specifically, the dysfunctional beliefs that are inputs in the RCT decision tree—and avoidance. They describe a vicious cycle: fear learning establishes a conditioned fear, which leads to anxious avoidance of the conditioned stimulus. The person develops negative beliefs about the CS which, in the absence of actual exposure to the CS, are never challenged or disconfirmed. These negative beliefs in turn inform the person’s decision-tree for specific choices related to the CS, creating anxious worry. Anxious worry, as an emotional state, negatively biases the options the anxious person believes they have. As a result, the person continues to avoid the CS, and continues to miss out on any opportunity to extinguish the conditioned fear and break the negative cycle (58,59).
The preceding argument suggests that avoidance is not only a salient behavioral symptom of anxiety disorders, but a keystone in its maintenance and continuation; therefore, it needs to be a key target in therapy and not viewed as merely a symptom. Both the RCT and Fear Learning paradigms provide avenues for doing so. RCT suggests the use of “behavioral experiments,” in which the patient actively seeks out information that may confirm or disconfirm existing beliefs about the utility or probability of certain outcomes (60). Max’s therapist might suggest that he talk to other students about what happened when they failed a test as a way to challenge his own belief about the consequences of failing. By doing so, he can update the values in his decision tree and perhaps begin to view his own prospects with less pessimism. Alternatively, the Fear Learning paradigm, which informs exposure-based therapy, also helps to clarify the conditions under which such therapy will not be effective. For example, exposure-based therapy may fail when patients engage in excessive discrimination, which has also been called “overaccommodation” (58). In overaccommodation, the patient focuses on particularities of the exposure situation that differentiate it from the ‘actual’ feared situation, and resultingly the patient fails to learn the intended message from the exposure (i.e., the patient fails to extinguish the conditioned response). In this scenario, rather than continuing with a purely exposure-based approach, the clinician might instead need to start by addressing the patient’s rate of discrimination before the exposure-based therapy can be successful.
Summary and conclusions
Anxiety disorders in children and adolescents are a major source of psychological impairment. A decision-making model of anxiety helps to explain the etiology, presentation, and maintenance of these disorders in terms of aberrant decision parameters that feed into ordinary, non-pathological human decision-making processes. In the RCT framework, anxious individuals stand out by their extreme utility- or probability-weightings for aversive outcomes and the worrying which results from feeling surrounded by negatively biased choices. The Fear Learning paradigm explains the establishment of conditioned fear responses, which become pervasive in anxious individuals due to a hyperactive generalization tendency and/or a lowered conditioning threshold, and result in anxious avoidance.
Assessment of pediatric anxiety disorders is a multi-step process that must draw on screening tools followed by more specific questionnaires in addition to a thorough interview about the patient’s experiences and history, as well as parent/caretaker input, and, when appropriate, teacher input. During the assessment clinicians should be sensitive to possible trauma exposure and its impact on the youth’s presentation. For mild-to-moderately severe presentations, CBT is the first line of recommended treatment. Where symptoms are severe, CBT should be combined with medication as the first line treatment. Medications are also indicated when CBT is not working or is inaccessible. Certain antidepressants show efficacy for treating pediatric anxiety disorders, whereas benzodiazepines and other anxiolytics do not. Finally, the decision-making model of anxiety suggests that current treatment modalities can be enhanced by directly targeting the aberrant parameters that distinguish anxious individuals from their non-anxious peers. That is, this model suggests the need for methods that alter extreme utility and probability beliefs, suppress the generalization tendency, and raise the conditioning threshold. In summary, when correctly assessed pediatric anxiety disorders can be effectively treated using current therapies and medication. Innovations based on decision parameters will further improve the treatments and reduce the suffering caused by these pervasive disorders.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Danielle Laraque-Arena and Ruth E. K. Stein) for the series “Integrating Mental Health in the Comprehensive Care of Children and Adolescents: Prevention, Screening, Diagnosis and Treatment” published in Pediatric Medicine. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://pm.amegroups.com/article/view/10.21037/pm-21-38/coif). The series “Integrating Mental Health in the Comprehensive Care of Children and Adolescents: Prevention, Screening, Diagnosis and Treatment” was commissioned by the editorial office without any funding or sponsorship. LA reports funding on a number of NIH grants, none of which were involved in the writing of this paper. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
1Reference for this entire section, unless cited otherwise, is American Psychiatric Association (2013).
References
- Mehta S, Farina A. Is being “sick” really better? Effect of the disease view of mental disorder on stigma. J Soc Clin Psychol 1997;16:405-19. [Crossref]
- Elster J. Rational Choice Theory: Cultural Concerns. Int Encycl Soc Behav Sci. 2001;12763-8.
- Thaler RH. Quasi rational economics. Russell Sage Foundation; 1994.
- Kahneman D. Thinking, fast and slow. Farrar, Straus And Giroux; 2011.
- LeDoux JE, Pine DS. Using neuroscience to help understand fear and anxiety: A two-system framework. Am J Psychiatry 2016;173:1083-93. [Crossref] [PubMed]
- Merikangas KR, He J, Burstein M, et al. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 2010;49:980-9. [Crossref] [PubMed]
- Barlow DH. Anxiety and its disorder: The nature and treatment of anxiety and panic. Guilford; 2004.
- Crocq MA. The history of generalized anxiety disorder as a diagnostic category. Dialogues Clin Neurosci 2017;19:107-16. [Crossref] [PubMed]
- Hofmann SG, Hay AC. Rethinking avoidance: Toward a balanced approach to avoidance in treating anxiety disorders. J Anxiety Disord 2018;55:14-21. [Crossref] [PubMed]
- Mayo Clinic. Anxiety disorders: Symptoms and causes [Internet]. Mayo Clinic. 2018. Available online: https://www.mayoclinic.org/diseases-conditions/anxiety/symptoms-causes/syc-20350961
- Savage LJ. The foundation of statistics. 2nd ed. Dover Publications, Inc.; 1972.
- Muris P, van der Heiden S. Anxiety, depression, and judgments about the probability of future negative and positive events in children. J Anxiety Disord 2006;20:252-61. [Crossref] [PubMed]
- Bishop SJ, Gagne C. Anxiety, depression, and decision making: A computational perspective. Annu Rev Neurosci 2018;41:371-88. [Crossref] [PubMed]
- Hartley CA, Phelps EA. Anxiety and Decision-Making. Biol Psychiatry 2012;72:113-8. [Crossref] [PubMed]
- Coon D. Introduction to psychology: gateways to mind and behavior. 12th ed. Cengage Learning; 2008.
- Watson JB, Rayner R. Conditioned emotional reactions. J Exp Psychol 1920;3:1-14. [Crossref]
- Miltenberger RG. Behavior modification: principles and procedures. Cengage Learning; 2016.
- Duits P, Cath DC, Lissek S, et al. Updated meta-analysis of classical fear conditioning in the anxiety disorders. Depress Anxiety 2015;32:239-53. [Crossref] [PubMed]
- Gao Y, Li W, Sui B, Abumaria N. Individual differences in learning rate and fear response predict fear memory and recovery in mice and human subjects. Neurosci Bull 2020;36:815-20. [Crossref] [PubMed]
- Dunne G, Reynolds G, Askew C. Stimulus fear relevance and the speed, magnitude, and robustness of vicariously learned fear. Behav Res Ther 2017;95:1-18. [Crossref] [PubMed]
- Gershman SJ, Hartley CA. Individual differences in learning predict the return of fear. Learn Behav 2015;43:243-50. [Crossref] [PubMed]
- Hein TP, de Fockert J, Ruiz MH. State anxiety biases estimates of uncertainty and impairs reward learning in volatile environments. NeuroImage 2021;224:117424. [Crossref] [PubMed]
- Browning M, Behrens TE, Jocham G, et al. Anxious individuals have difficulty learning the causal statistics of aversive environments. Nat Neurosci 2015;18:590-6. [Crossref] [PubMed]
- Dymond S, Dunsmoor JE, Vervliet B, et al. Fear generalization in humans: Systematic review and implications for anxiety disorder research. Behav Ther 2015;46:561-82. [Crossref] [PubMed]
- Stegmann Y, Schiele MA, Schümann D, et al. Individual differences in human fear generalization—pattern identification and implications for anxiety disorders. Transl Psychiatry 2019;9:307. [Crossref] [PubMed]
- Lissek S, Kaczkurkin AN, Rabin S, et al. Generalized Anxiety Dsorder is associated with overgeneralization of classically conditioned fear. Biol Psychiatry 2014;75:909-15. [Crossref] [PubMed]
- Lissek S, Rabin S, Heller RE, et al. Overgeneralization of conditioned fear as a pathogenic marker of panic disorder. Am J Psychiatry 2010;167:47-55. [Crossref] [PubMed]
- Kaczkurkin AN, Burton PC, Chazin SM, et al. Neural substrates of overgeneralized conditioned fear in PTSD. Am J Psychiatry 2017;174:125-34. [Crossref] [PubMed]
- El-Bar N, Laufer O, Yoran-Hegesh R, et al. Over-generalization in youth with anxiety disorders. Soc Neurosci 2017;12:76-85. [Crossref] [PubMed]
- Dibbets P, van den Broek A, Evers EAT. Fear conditioning and extinction in anxiety- and depression-prone persons. Memory 2015;23:350-64. [Crossref] [PubMed]
- Wong AHK, Pittig A. Costly avoidance triggered by categorical fear generalization. Behav Res Ther 2020;129:103606. [Crossref] [PubMed]
- Jellinek MS. Screening for psychosocial disorders in pediatric practice. Am J Dis Child 1988;142:1153. [PubMed]
- Birmaher B, Khetarpal S, Brent D, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry 1997;36:545-53. [Crossref] [PubMed]
- The research units on pediatric psychopharmacology anxiety study group. The Pediatric Anxiety Rating Scale (PARS): Development and Psychometric Properties. J Am Acad Child Adolesc Psychiatry 2002;41:1061-9. [Crossref]
- March JS, Parker JDA, Sullivan K, et al. The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry 1997;36:554-65. [Crossref] [PubMed]
- Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol 1959;32:50-5. [Crossref] [PubMed]
- Beck AT, Epstein N, Brown G, et al. An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol 1988;56:893-7. [Crossref] [PubMed]
- Norman SB, Hami Cissell S, Means-Christensen AJ, et al. Development and validation of an Overall Anxiety Severity And Impairment Scale (OASIS). Depress Anxiety 2006;23:245-9. [Crossref] [PubMed]
- Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing Generalized Anxiety Disorder. Arch Intern Med 2006;166:1092. [Crossref] [PubMed]
- Mossman SA, Luft MJ, Schroeder HK, et al. The Generalized Anxiety Disorder 7-item (GAD-7) scale in adolescents with generalized anxiety disorder: signal detection and validation. Ann Clin Psychiatry 2017;29:227-34A. [PubMed]
- Domschke K, Maron E. Genetic factors in anxiety disorders. Mod Trends Pharmacopsychiatry 2013;29:24-46. [Crossref] [PubMed]
- Meier SM, Deckert J. Genetics of anxiety disorders. Curr Psychiatry Rep 2019;21:16. [Crossref] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
- Gandhi B, Cheek S, Campo JV. Anxiety in the pediatric medical setting. Child Adolesc Psychiatr Clin N Am 2012;21:643-53. [Crossref] [PubMed]
- Wilbur C, Bitnun A, Kronenberg S, et al. PANDAS/PANS in childhood: Controversies and evidence. Paediatr Child Health 2019;24:85-91. [Crossref] [PubMed]
- Freidl EK, Stroeh OM, Elkins RM, et al. Assessment and treatment of anxiety among children and adolescents. FOCUS 2017;15:144-56. [Crossref] [PubMed]
- Beck JS. Cognitive Behavior Therapy: basics and beyond. 2nd ed. The Guilford Press; 2011.
- Seligman LD, Ollendick TH. Cognitive Behavioral Therapy for anxiety disorders in youth. Child Adolesc Psychiatr Clin N Am 2011;20:217-38. [Crossref] [PubMed]
- Banneyer KN, Bonin L, Price K, et al. Cognitive Behavioral Therapy for childhood anxiety disorders: a review of recent advances. Curr Psychiatry Rep 2018;20:65. [Crossref] [PubMed]
- Connolly SD, Bernstein GA. Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry 2007;46:267-83. [Crossref] [PubMed]
- Strawn JR, Geracioti L, Rajdev N, et al. Pharmacotherapy for generalized anxiety disorder in adult and pediatric patients: An evidence-based treatment review. Expert Opin Pharmacother 2018;19:1057-70. [Crossref] [PubMed]
- Strawn JR, Prakash A, Zhang Q, et al. A Randomized, Placebo-Controlled Study of Duloxetine for the Treatment of Children and Adolescents With Generalized Anxiety Disorder. J Am Acad Child Adolesc Psychiatry 2015;54:283-93. [Crossref] [PubMed]
- Stewart SE. About medications for pediatric OCD [Internet]. OCD in Kids. Available online: https://kids.iocdf.org/professionals/mh/meds-for-pediatric-ocd/
- Strawn JR, Welge JA, Wehry AM, et al. Efficacy and tolerability of antidepressants in pediatric anxiety disorders: a systematic review and meta-analysis. Depress Anxiety 2015;32:149-57. [Crossref] [PubMed]
- Wang Z, Whiteside SPH, Sim L, et al. Comparative Effectiveness and Safety of Cognitive Behavioral Therapy and Pharmacotherapy for Childhood Anxiety Disorders: A Systematic Review and Meta-analysis. JAMA Pediatr 2017;171:1049-56. [Crossref] [PubMed]
- Ipser JC, Stein DJ, Hawkridge S, et al. Pharmacotherapy for anxiety disorders in children and adolescents. Cochrane Database Syst Rev 2009;8:CD005170. [Crossref] [PubMed]
- Borza L. Cognitive-behavioral therapy for generalized anxiety. Dialogues Clin Neurosci 2017;19:203-8. [Crossref] [PubMed]
- Moutoussis M, Shahar N, Hauser TU, et al. Computation in psychotherapy, or how computational psychiatry can aid learning-based psychological therapies. Comput Psychiatr 2018;2:50-73. [Crossref] [PubMed]
- Pearson RM, Heron J, Button K, et al. Cognitive styles and future depressed mood in early adulthood: The importance of global attributions. J Affect Disord 2015;171:60-7. [Crossref] [PubMed]
- Rouf K. Oxford Guide to Behavioural Experiments in Cognitive Therapy. Bennett-Levy J, Butler G, Fennell M, et al, editors. Oxford, England: Oxford University Press, 2004.
Cite this article as: Amsel L, Kortenhorst J. Understanding adolescent anxiety disorders through the lens of decision science: towards a mathematical psychiatry. Pediatr Med 2022;5:16.

