
Mediational models of maternal stress in neonatal intensive care units
Introduction
Hans Selye defined stress as an organism’s ability to respond to surrounding stressors or events that threaten its homeostasis (1). Lecic-Tosevski et al. (2) distinguishes stress as not only relating to physical and/or physiologic stressors, but also to the degree in which situations are “determined by one’s perception of their stressfulness” (3). Such subjectivity is a function of recipients’ disposition, traits, and their environment, e.g., resilience/vulnerability, coping skills, life experiences, mental state, age (2). Together, these attributes determine the “tolerance” level that an individual has in managing a situation he/she is confronting at a particular time in life. As such, whether a stressor is truly ‘threatening’ will depend on our “response intensity or magnitude” to that event with the latter determining our behavioral and/or emotional response.
In the field of Ecology, the use of the Multiple-Stressor modeling approach has gained in popularity. Indeed, researchers have long recognized how the simultaneous interactions of multiple stressors onto an organism could lead to uncertain outcomes as the multitude of potential combinations between these stressors, be they beneficial or detrimental, makes it difficult to predict any likely outcome. As such, not only is it difficult to identify a potential impact on a particular organism, but more importantly, how to best resolve the problem (4,5). Although Multiple-Stressor research is a recognized theoretical framework in understanding stressful impacts on environmental or ecological adaptations, it has not yet received the attention it deserves in the study of stress adaptation/behaviors in humans (6-9). Hale and al. argue that although animals/humans respond behaviorally to individual stressors, it is unclear to what extent the complex interactions of these stressors amongst themselves further contribute to a responder’s overall behaviors (8). As such, to better understand human behavioral responses to multiple stressors, a more appropriate approach would be to quantify behavioral responses not only in terms of the impact of the stressors themselves, but also of their interactions, be they synergistic or antagonistic, with each other along with the recipients’ attributes.
Maternal stress in neonatal intensive care units (NICU)
With the sustained increase in the survival of preterm infants over the last three decades, parental stress following the birth of a child is undeniable. This is evidenced by the extensive research literature in this domain be they in reviews or studies focused on particular infant’s characteristics, parental distress, e.g., depression, anxiety, or imbalanced family situations (10-27). Of interest, studies have shown how such parental stress responses may be associated with a particular condition observed in their infant(s). For instance, Gordo et al. in a study conducted on full-term infants identified an association between parental depression and their perceived parenting competence in the care of their child (28). Musabirema et al. observed that parental perception of stress during their infants’ NICU hospitalization was most impacted by their baby’s looks and behavior as monitored by the Parental Stressor Scale:NICU (29,30).
Currently, well-defined intervention protocols for NICU parents are limited (23,31-36). In a systematic review and meta-analysis monitoring NICU parental distress in 1,643 controlled studies published before 2017, the authors concluded that “NICU interventions modestly reduced parental distress” (37). Importance of identifying risk factors for early interventions are critical because the initiation of maternal behavior/motherhood requires the continuous interfacing between mother and child(ren). With the global recognition that “mother’s milk is best”, breastfeeding support and milk banks availability throughout NICUs have expanded (38-40). However, of importance, it is the appropriate initiation of mother-infant interactions that will ultimately determine their breastfeeding success and the nature of their bond/attachment (41-45). As NICU hospitalization may become a traumatic experience for both infants and parents, a “trauma-informed” care approach has been recommended between parents and staff to emphasize safety, trustworthiness/transparency, peer support, mutuality, parents and staff empowerment, as well as cultural/historical/gender concerns (46). This brief review of the multitude of differing challenges facing mothers in the NICU illustrates the difficulty facing providers when assisting parents through their infants’ hospitalization. This is further exacerbated by the fact that NICU care providers are trained to care for a pediatric population and their parents are not their patients per se.
At present, studies on maternal stress in NICU have focused primarily on alleviating recognized psychological issues such as depression, anxiety (17,27,45,47,48). However, as interactions between multiple stressors may further impact behaviors and maternal mental health, our understanding of the “overall” stress experienced by mothers and the current support we offer is incomplete. There is limited research examining how the stress experienced by mothers in NICUs arise. It is normally reasoned that maternal “response intensity” to postpartum depression/anxiety, for example, results from their personal traits (20,49,50). If correct, given the broad spectrum of “personalities” in our society, one cannot expect that only a “one size fits all” care approach would suffice. Indeed, individuals’ attributes such as personality and external socioeconomic factors would contribute to their perception of how stressful their personal situation is.
As the complexity of the stress experienced by mothers in NICUs parallels the environmental perturbations occurring in natural ecological systems, it is hypothesized that the theoretical Multiple-Stressor framework used by environmental researchers can allow for the development of similar mediational models of specific maternal stress outcomes. If this could be attained, it would be expected that such approach would lead to the development of more effective programs to assist individual NICU mothers as it will offer caregivers a clearer grasp of the varied stressors they are confronting as a function of their respective attributes and socioeconomic environment. Thus, the goal of the present study was to identify maternal attributes that could lead to the development of maternal Multiple-Stressors mediational models. The following models were examined: Depression, Anxiety, NICU Stress, Perceived Social Support, and Coping Skills.
We present the following article in accordance with the MDAR reporting checklist (available at https://pm.amegroups.com/article/view/10.21037/pm-21-35/rc).
Methods
Subjects
Thirty mothers of infants born between 24 and 29 weeks gestation were recruited from a convenient cross-sectional sample of a large prospective study conducted between August 2005 and July 2011 in the NICUs at Texas Children’s Hospital, Baylor College of Medicine (Houston, TX, USA). This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by the Baylor College of Medicine Internal Review Board (H-18036). Written consent form was obtained from mothers.
Assessment of maternal socioeconomic characteristics and psychological traits
Mothers were recruited at least 2 weeks postpartum to ensure that their infants were clinically stable. At that time, social-economic characteristics were collected, e.g., race/ethnicity, age, education, income. Because race is primarily based on one’s physical/genetic attributes and ethnicity describes one’s cultural expression/tradition, these two descriptors were combined as individuals in our current society may identify themselves through a racial or ethnic background. At the same time, to monitor maternal attributes, mothers responded to the following standard self-reported instruments (Table 1). The Affect Intensity Measure (AIM) monitors the intensity of positive or negative emotions experienced by individuals; the higher the score, the greater their emotional response (51). The Crowne-Marlowe Social Desirability Scale (CM) was used to assess subjects’ “social desirability” trait or their need for social approval or avoidance of social disapproval (52,57). It measures subjects’ response bias to self-reported psychological questionnaires; the higher the score, the more likely the subjects will respond towards social approval and the lower the score, the more “truthful” the respondents. This measure was used as a covariate in data analyses. The Edinburgh Postnatal Depression Scale (EPDS) monitored maternal depression (53); the higher the score, the greater the depression. The Brief Symptom Inventory is a screening questionnaire that assesses nine adult symptom dimensions, i.e., somatization, obsession-compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism, and calculates a Global Severity Index, Positive Symptoms Total, and Positive Symptom Distress Index. In this report, only the Anxiety dimension was used [BSI-Anx; Pearsonassessments.com; (54)]. The Parental Stress Scale:NICU monitored maternal stress pertaining to the sight and sounds in the NICU, baby’s looks, parenting role alteration or parental alteration due to their inability to care for their infant as a parent, and their ease in communicating with NICU staff (29). The Multidimensional Scale of Perceived Social Support or Perceived Social Support (MSPSS) was used to evaluate the subjects’ perceived stress from family, friends, and significant other (55). The Coping Inventory for Stressful Situations (CISS) differentiated between task-oriented (CISS-Task), emotion-oriented (CISS-Emotion), and avoidance-oriented (CISS-Avoidance) coping skills that individuals may use in handling a difficult event (56). For individuals who are task-oriented, the higher their score, the more likely they will use behavioral or cognitive problem-solving techniques, emotion-oriented individuals will more likely respond with emotional outbursts, self-preoccupation, while avoidance-oriented counterparts will rely on self-distraction with other activities or social diversion. Maternal postpartum health was monitored by the number of postpartum visits mothers had with their own health provider.
Table 1
| Tests | To evaluate |
|---|---|
| Affect Intensity Measure (AIM) (51) | • Trait characterizing an individual’s magnitude of emotional response (the higher the score, the greater the emotional response) |
| Crowne-Marlowe Social Desirability Scale (CM) (52) | • Trait characterizing an individual’s |
| -Inclination to be viewed favorably by others | |
| -Truthfulness of responses | |
| (the lower the score, the more truthful the response) | |
| Edinburgh Postnatal Depression Scale (EPDS) (53) | • Postpartum depression (the higher the score, the greater the depression) |
| Brief Symptom Inventory Anxiety (BSI-Anx) (54) | • Anxiety (the higher the score, the greater the anxiety) |
| Parental Stress Scale:NICU (PSS:NICU) (29) | • Perceived stress in the NICU resulting from: |
| -Sights (53) & sounds in NICU (S&S) | |
| -Baby’s looks/behaviors (Looks) | |
| -Parenting alteration (Parent) | |
| -Staff communication (Staff) | |
| (the higher the scores, the more stressful these factors) | |
| Multidimensional Scale of Perceived Social Support (MSPSS) (55) | • Perceived social support (the higher the score, the greater the perceived social support) |
| Coping Inventory for stressful Situations (CISS) (56) | • Task-oriented coping (CISS-Task) |
| • Emotion-oriented coping (CISS-Emotion) | |
| • Avoidance-oriented coping (CISS-Avoidance) | |
| Maternal health condition | • Number of visits to healthcare providers |
Maternal mediational stress models
The following mediational models were considered: Depression; Anxiety; the stress of NICU sights and sounds, baby’s looks, parental alteration, and staff communications; Perceived Social Support; and Task-oriented/Emotion-oriented/Avoidance-oriented coping skills.
Statistical analyses
One-way ANOVA was used to compare maternal characteristics and psychological measures by race/ethnicity (Figure 1, Table 2).
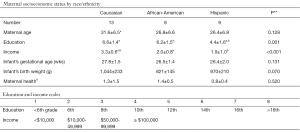
Table 2
| Maternal psychological measures | Caucasian | African-American | Hispanic | P* |
|---|---|---|---|---|
| Affect intensity measure (AIM) | 3.6±0.4# | 3.8±0.6 | 3.93±0.5 | 0.465 |
| Crowne-Marlowe Social Desirability Scale (CM) | 16.5±5.8a,b | 26.4±4.2a | 22.3±4.2b | 0.001 |
| Postpartum depression (EPDS) | 10.9±4.7 | 11.6±6.2 | 13.5±5.5 | 0.546 |
| Anxiety (BSI-Anx) | 57.3±12.3 | 52.9±8.4 | 48.9±11.5 | 0.297 |
| Parental Stress Scale:NICU (PSS:NICU) | ||||
| Sight & Sound | 3.1±0.7 | 2.5±1.2 | 2.3±1.3 | 0.268 |
| Baby’s Looks | 3.4±0.7 | 2.9±1.2 | 3.3±1.1 | 0.479 |
| Parenting Alteration | 4.3±0.9 | 4.1±1.1 | 3.9±1.2 | 0.736 |
| Staff Communication | 2.2±1.0 | 1.5±0.6 | 1.7±0.9 | 0.252 |
| Perceived Social Support (MSPSS) | 6.5±0.5 | 5.5±1.3 | 6.2±0.9 | 0.084 |
| Coping Inventory for Stressful Situations (CISS) | ||||
| Task-oriented (CISS-Task) | 49.7±15.1 | 56.0±8.6 | 45.0±10.8 | 0.273 |
| Emotion-oriented (CISS-Emotion) | 48.0±9.4 | 47.4±11.1 | 48.5±12.2 | 0.980 |
| Avoidance-oriented (CISS-Avoidance) | 46.5±11.4a | 59.4±12.5a | 47.8±10.8 | 0.060 |
#, Mean ± SD; *, One-way ANOVA; a,b, Post hoc Fisher LSD: P<0.05 between symbols.
To build a mediational model for assessing the potential interactions between maternal attributes, as measured by the self-reported psychological instruments, and a particular maternal stress outcome model, multiple regression analyses were first conducted to identify the maternal attributes significantly associated (P<0.05) with each model of stress outcomes. Following this first step, the ‘Best Subsets Regression’ analysis (www.minitab.com) was used to identify the 4 maternal variables that best correlated with the models of interest. Unlike a stepwise approach whereby a specific set of predictors are added or removed based on their combined statistical significance to result in a single regression model, the Best Subsets approach compared all possible models using the set of maternal predictors identified in the original multiple regression analyses and displays the ‘best-fitting’ models in order of highest to lowest adjusted R2 and/or Mallows’Cp close to the number of predictors of interest (in our case 4) to help users choose a final model.
Results
There was no significant difference in maternal socioeconomic status and psychological outcomes between Race/Ethnicity except for Education and Income (P≤0.001; Figure 1) and Crowne-Marlowe Social Desirability Scale between Caucasians and African-American mothers (CM; P=0.001; Table 2). As mentioned in an earlier study (45), the latter observation emphasizes the importance in studies using self-reported testing to consider the truthfulness of respondents as it is critical to researchers’ ability to conduct accurate studies (45,58-60). As maternal postpartum visits to their own care provider were minimal, it is presumed that our observations were not impacted by mothers’ concern over their own health.
Table 3 presents the individual maternal attributes associated with the different mediational stress models. In Table 4, the 4 maternal attributes that best correlated with each of the mediational stress models are presented. In each of these models, they are listed from their highest to lowest individual P values, be they statistically significant (P<0.05) or not (P>0.05, NS) along with their positive (+) or negative (−) correlation with the respective models. The % adjusted R2 shows the effect that these 4 predictors together contributed to the original multiple regression analyses. The overall P value is that of the original multiple regression analyses. It is emphasized that this approach does not necessarily identify a ‘best’ interactive model, but rather allows users to select an ‘optimal’ model based on their knowledge of the subject area under study (https://support.minitab.com/en-us/minitab-express/1/help-and-how-to/modeling-statistics/regression/how-to/best-subsets/before-you-start/overview/).
Table 3
| Maternal attributes* | Mediational models of maternal stress outcomes | |||
|---|---|---|---|---|
| Race/Ethnicity | Depression | NICU Baby’s Looks | NICU Parenting Alteration | |
| Income | Anxiety | NICU Baby’s Looks | NICU Staff Communication | Use of Avoidance-oriented coping skill |
| Education | NICU Sight & Sounds | Use of Task-oriented coping skill | ||
| AIM | Anxiety | PSS:NICU Sight & sounds | Use of Avoidance-oriented coping skill | |
| CM | NICU Sight & sounds | Perceived Social Support | Use of Emotion-oriented coping skill | |
| EPDS | NICU Parenting Alteration | NICU Staff Communication | Use of Emotion-oriented coping skill | |
| BSI-Anx | NICU Parenting Alteration | Use of Task-oriented coping skill | Use of Avoidance-oriented coping skill | |
| PSS:NICU (Sight & Sounds) | NICU Staff Communication | |||
| PSS:NICU (Baby’s Looks) | NICU Sight & sounds | NICU Parenting Alteration | Use of Emotion-oriented coping skill | |
| PSS:NICU (Parenting Alteration) | Depression | NICU Baby’s Looks | ||
| PSS:NICU (Staff Communication) | Depression | |||
| MSPSS | Depression | Use of Task-oriented coping skill | ||
| CISS-Task | Anxiety | Perceived Social Support | Use of Avoidance-oriented coping skill | |
| CISS-Emotion | Depression | NICU Baby’s Looks | NICU Staff Communication | Perceived Social Support |
| CISS-Avoidance | Anxiety | Use of Task-oriented coping skill | ||
*, Maternal Attributes identified by respective self-reported psychological instruments; AIM, Affect Intensity Measure; CM, Crowne-Marlowe Social Desirability Scale; EPDS, Edinburgh Postnatal Depression Scale; BSI-Anx, Brief Symptom Inventory-Anxiety; PSS:NICU, Parental Stress Scale: NICU; MSPSS, Multidimensional Scale of Perceived Social Support.
Table 4
| Maternal stress outcomes models | Combined 4 maternal attributes contributing best to each mediational model | R2 (adj) % | P* (overall) | |||
|---|---|---|---|---|---|---|
| Depression | Parent Alteration (+)# (<0.001)§ | CISS-Emotion (+) (0.001) | Race/Ethnicity (0.002) | Perceived Stress (-) (0.006) | 73 | <0.001 |
| Anxiety | Income (+) (<0.001) | CISS-Task (-) (0.001) | CISS-Avoidance (+) (0.004) | AIM (-) 0.021) | 56 | 0.001 |
| NICU Sights & Sounds | Baby’s Looks (+) (0.012) | Social Desirability (-) (0.020) | Education (+) (0.028) | AIM (+) (0.049) | 53 | <0.001 |
| NICU Stress (Baby’s Looks) | Parenting Alteration (+) (<0.001) | Income (+) (0.006) | Race/Ethnicity (0.008) | CISS-Emotion (-) (0.121/NS) | 72 | <0.001 |
| NICU Stress (Parenting Alteration) | Baby’s Looks (+) (<0.001) | Race/Ethnicity (0.002) | EPDS (+) (0.003) | BSI-Anx (-) (0.386/NS) | 71 | <0.001 |
| NICU Stress (Staff Communication) | EPDS (+) (0.020) | Income (+) (0.075/NS) | CISS-Emotion (-) (0.088/NS) | Sights & Sounds (+) (0.197/NS) | 41 | 0.006 |
| Perceived Social Support | CM (-) (<0.001) | CISS-Emotion (-) (0.008) | CISS-Task (+) (0.032) | AIM (+) (0.092/NS) | 52 | 0.001 |
| Coping Skills (Task-oriented) | Education (+) (0.002) | BSI-Anx (-) (0.002) | Perceived Social Support (+) (0.010) | CISS-Avoidance (+) (0.026) | 58 | <0.001 |
| Coping Skills (Emotion-oriented) | EPDS (+) (0.001) | CM (-) (0.024) | Baby’s Looks (-) (0.062/NS) | AIM (+) (0.369/NS) | 45 | 0.002 |
| Coping skills (Avoidance-oriented) | Income (-) (<0.001) | AIM (+) (<0.001) | CISS-Task (+) (<0.001) | BSI-Anx (+) (0.004) | 65 | <0.001 |
#, (+) positive and (-) negative correlation with corresponding Maternal Stress Models; §, individual maternal traits with significant (P<0.05) and non-significant P values (>0.05; NS) within each mediational model; *, overall P value of the original multiple regression analysis for individual mediational models; AIM, Affect Intensity Measure; CM, Crowne-Marlowe Social Desirability Scale; EPDS, Edinburgh Postnatal Depression Scale; BSI-Anx, Brief Symptom Inventory-Anxiety; PSS:NICU, Parental Stress Scale: NICU; MSPSS, Multidimensional Scale of Perceived Social Support.
Discussion
From the literature review briefly summarized above, it is evident that mothers experience a broad “variety” of stressors during their baby’s NICU hospitalization. Along with the stress of having given birth to a premature fragile infant, mothers must confront not only their immediate apprehension of what can happen to their baby(ies), but also their personal daily life challenges. As such, the cumulative risks they experience becomes difficult to gage as it requires identifying not only concerns over their infant(s), but also the impact of how their personality and lifestyle may contribute to their overall NICU experience. On such bases, it may not be surprising that, currently, encouraging mothers to maintain breastfeeding, skin-to-skin contact, or frequent visits to the NICU is often unpredictable.
With the realization that when an individual simultaneously faces multiple stressors, the overall impact he/she experiences becomes difficult to assess as it is not only the resultant of individual stressors themselves, but also of their interactions with each other. Thus, identification of a main “culprit” becomes difficult and any intervention/support aimed at a particular stressor, e.g., depression, anxiety, may not lead to any significant benefit. Given that the current assistance mothers receive in the NICU are deemed to only “modestly” reduce their distress (37), the present exploratory study was initiated to determine whether the Multiple-Stressor theoretical modeling framework, validated by ecologists, could be also applicable to the human paradigm, as the similarities existing between the stressors NICU mothers are exposed to parallel those of organisms in the environment (4,5,7). In addition, the availability of the Best Subset Regression technique offered the opportunity to, not only, identify the stressors implicated in particular stress models, but also to monitor statistically their combined impact on maternal stressors. As such, it is advanced that the combined use of these two techniques can offer NICU care providers a more comprehensive psychosocial understanding of the struggle these mothers face. It is expected that such understanding will allow psychosocial therapists to develop more efficacious support for their mothers as any treatment benefits could be verified by repeated psychological re-evaluation over time. For instance, it is advanced that within the Depression mediational model (Table 4), based on the maternal attributes identified, if support were offered to reduce mothers’ stress for their inability to be a parent (parental alteration), emotion-oriented outbursts (CISS-Emotion), and perception of lack of social support (Perceived Social Support), maternal overall Depression would be decreased. A “chain reaction” resulting from such improved maternal attributes and overall maternal Depression will additionally lead to a decrease in the intensity of the other stressors who are associated with the same maternal attributes. In our example, as overall Depression, parental alteration, CISS-Emotion, and Perceived Social Support are improved, the stress ensuing from one’s Baby’s Looks via parenting alteration, staff communication via CISS-Emotion, and CISS-Task via Perceived Social Support would be expected to be improved as well. This example illustrates the outreaching impact that such an approach can have due to the normal interactions existing between stressors.
Used in conjunction with maternal support programs (61) under the guidance of social workers/psychotherapists, this analytical approach may help mothers better understand and manage their personal struggles. The latter can be very validating and powerful for parental adaptation and behavioral changes. It would not only benefit parents’ personal wellbeing, but also increase their NICU participation in the care of their babies. It is important to remember that parental stress in the NICU does not only pertain to mothers, but also fathers. As such, proper assistance for both parents would be essential to fully support the long-term development of appropriate parent-child dyads in NICUs as well as home (35,44,45,62-68).
In summary, this study explored the applicability of the Multiple Stressor modeling commonly used by ecologists to human studies. Along with the use of the Best Subset Regression analyses, it has been possible to develop statistical mediational models of stressors that were not only associated with differing maternal attributes, but also identify their synergistic/antagonistic interactions. This emphasizes the clinical importance of considering not only individual maternal traits, but also their interactions with each other when assisting parents.
Conclusions
To our knowledge, this is the first study that uses the Multiple-Factor modeling approach to decipher the complex multi-factorial interactions facing mothers following a premature delivery. It is advanced that identification of such key components and their respective interactions with each other will provide a better informed approach to the development of appropriate interventions to alleviate the stress of NICU mothers. If mothers were to receive a more comprehensive psychosocial support that helps identify their personal characteristics/traits most affected in their NICU experience, better focused and individualized support could be offered for their care.
Study limitations/clinical implications/future directions
Due to the exploratory nature of this work, subjects’ sample size may appear of concern. However, the observations collected validate the Multiple-Stressor modeling approach as they demonstrated statistically significant associations between maternal traits and NICU-generated stressors. Our results support the notion that such analytical approach could be of great value to clinical researchers and clinicians as it offers the ability to identify, monitor, and support the various personality traits most at risk in parents of NICU infants.
Acknowledgments
The authors wish to thank their many mothers who did not hesitate to participate in our study. The authors are grateful to their research staff who tirelessly ensured the success and completion of this study.
Funding: This study was supported by the National Institutes of Health (NIH Research Project Grant R01 HD 44469): “Oral Feeding in Infants”.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Steven M. Barlow) for the series “Neonatal Feeding and Developmental Issues” published in Pediatric Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at https://pm.amegroups.com/article/view/10.21037/pm-21-35/rc
Data Sharing Statement: Available at https://pm.amegroups.com/article/view/10.21037/pm-21-35/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://pm.amegroups.com/article/view/10.21037/pm-21-35/coif). This study was supported by the National Institutes of Health (NIH Research Project Grant R01 HD 44469): “Oral Feeding in Infants”. The series “Neonatal Feeding and Developmental Issues” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by the Baylor College of Medicine Internal Review Board (H-18036) and consent was taken from all the subjects.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Selye H. The general adaptation syndrome and the diseases of adaptation. J Clin Endocrinol Metab 1946;6:117-230. [Crossref] [PubMed]
- Lecic-Tosevski D, Vukovic O, Stepanovic J. Stress and personality. Psychiatriki 2011;22:290-7. [PubMed]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385-96. [Crossref] [PubMed]
- Maher RL, Rice MM, McMinds R, et al. Multiple stressors interact primarily through antagonism to drive changes in the coral microbiome. Sci Rep 2019;9:6834. [Crossref] [PubMed]
- Piggott JJ, Townsend CR, Matthaei CD. Reconceptualizing synergism and antagonism among multiple stressors. Ecol Evol 2015;5:1538-47. [Crossref] [PubMed]
- Linder SH, Sexton K. Conceptual models for cumulative risk assessment. Am J Public Health 2011;101:S74-81. [Crossref] [PubMed]
- Orr JA, Vinebrooke RD, Jackson MC, et al. Towards a unified study of multiple stressors: divisions and common goals across research disciplines. Proc Biol Sci 2020;287:20200421. [Crossref] [PubMed]
- Hale R, Piggott JJ, Swearer SE. Describing and understanding behavioral responses to multiple stressors and multiple stimuli. Ecol Evol 2016;7:38-47. [Crossref] [PubMed]
- Goussen B, Price OR, Rendal C, et al. Integrated presentation of ecological risk from multiple stressors. Sci Rep 2016;6:36004. [Crossref] [PubMed]
- Forcada-Guex M, Borghini A, Pierrehumbert B, et al. Prematurity, maternal posttraumatic stress and consequences on the mother-infant relationship. Early Hum Dev 2011;87:21-6. [Crossref] [PubMed]
- Coppola G, Cassibba R, Costantini A. What can make the difference? Premature birth and maternal sensitivity at 3 months of age: the role of attachment organization, traumatic reaction and baby's medical risk. Infant Behav Dev 2007;30:679-84. [Crossref] [PubMed]
- Swain JE, Konrath S, Dayton CJ, et al. Toward a neuroscience of interactive parent-infant dyad empathy. Behav Brain Sci 2013;36:438-9. [Crossref] [PubMed]
- Neri E, Agostini F, Salvatori P, et al. Mother-preterm infant interactions at 3 months of corrected age: influence of maternal depression, anxiety and neonatal birth weight. Front Psychol 2015;6:1234. [Crossref] [PubMed]
- Tester-Jones M, O'Mahen H, Watkins E, et al. The impact of maternal characteristics, infant temperament and contextual factors on maternal responsiveness to infant. Infant Behav Dev 2015;40:1-11. [Crossref] [PubMed]
- Petit AC, Eutrope J, Thierry A, et al. Mother's Emotional and Posttraumatic Reactions after a Preterm Birth: The Mother-Infant Interaction Is at Stake 12 Months after Birth. PLoS One 2016;11:e0151091. [Crossref] [PubMed]
- Yaari M, Millo I, Harel-Gadassi A, et al. Maternal resolution of preterm birth from 1 to 18 months. Attach Hum Dev 2017;19:487-503. [Crossref] [PubMed]
- Zimmerman E, Lau C. The Development of the Mother-Infant Mutualistic Screening Scale. J Pediatr Mother Care 2017;2:107. [Crossref] [PubMed]
- Winter L, Colditz PB, Sanders MR, et al. Depression, posttraumatic stress and relationship distress in parents of very preterm infants. Arch Womens Ment Health 2018;21:445-51. [Crossref] [PubMed]
- Grunberg VA, Geller PA, Bonacquisti A, et al. NICU infant health severity and family outcomes: a systematic review of assessments and findings in psychosocial research. J Perinatol 2019;39:156-72. [Crossref] [PubMed]
- Montoya-Williams D, Passarella M, Grobman WA, et al. Racial/ethnic differences in maternal resilience and associations with low birthweight. J Perinatol 2021;41:196-203. [Crossref] [PubMed]
- Oyetunji A, Chandra P. Postpartum stress and infant outcome: A review of current literature. Psychiatry Res 2020;284:112769. [Crossref] [PubMed]
- Al Maghaireh DF, Abdullah KL, Chan CM, et al. Systematic review of qualitative studies exploring parental experiences in the Neonatal Intensive Care Unit. J Clin Nurs 2016;25:2745-56. [Crossref] [PubMed]
- Roque ATF, Lasiuk GC, Radünz V, et al. Scoping Review of the Mental Health of Parents of Infants in the NICU. J Obstet Gynecol Neonatal Nurs 2017;46:576-87. [Crossref] [PubMed]
- Montirosso R, Provenzi L, Calciolari G, et al. Measuring maternal stress and perceived support in 25 Italian NICUs. Acta Paediatr 2012;101:136-42. [Crossref] [PubMed]
- Garfield L, Holditch-Davis D, Carter CS, et al. Risk factors for postpartum depressive symptoms in low-income women with very low-birth-weight infants. Adv Neonatal Care 2015;15:E3-8. [Crossref] [PubMed]
- Bonacquisti A, Geller PA, Patterson CA. Maternal depression, anxiety, stress, and maternal-infant attachment in the neonatal intensive care unit. J Reprod Infant Psychol 2020;38:297-310. [Crossref] [PubMed]
- Lau C, Turcich MR, Smith EO. Early detection of parenting stress in mothers of preterm infants during their first-year home. BMC Psychol 2020;8:66. [Crossref] [PubMed]
- Gordo L, Oliver-Roig A, Martínez-Pampliega A, et al. Parental perception of child vulnerability and parental competence: The role of postnatal depression and parental stress in fathers and mothers. PLoS One 2018;13:e0202894. [Crossref] [PubMed]
- Miles MS, Funk SG, Carlson J. Parental Stressor Scale: neonatal intensive care unit. Nurs Res 1993;42:148-52. [Crossref] [PubMed]
- Musabirema P, Brysiewicz P, Chipps J. Parents perceptions of stress in a neonatal intensive care unit in Rwanda. Curationis 2015;38:1499. [Crossref] [PubMed]
- O'Brien K, Robson K, Bracht M, et al. Effectiveness of Family Integrated Care in neonatal intensive care units on infant and parent outcomes: a multicentre, multinational, cluster-randomised controlled trial. Lancet Child Adolesc Health 2018;2:245-54. [Crossref] [PubMed]
- Haward MF, Lantos J, Janvier A, et al. Helping Parents Cope in the NICU. Pediatrics 2020;145:e20193567. [Crossref] [PubMed]
- Chertok IR, McCrone S, Parker D, et al. Review of interventions to reduce stress among mothers of infants in the NICU. Adv Neonatal Care 2014;14:30-7. [Crossref] [PubMed]
- Treyvaud K, Spittle A, Anderson PJ, et al. A multilayered approach is needed in the NICU to support parents after the preterm birth of their infant. Early Hum Dev 2019;139:104838. [Crossref] [PubMed]
- Bry A, Wigert H. Psychosocial support for parents of extremely preterm infants in neonatal intensive care: a qualitative interview study. BMC Psychol 2019;7:76. [Crossref] [PubMed]
- Franck LS, O'Brien K. The evolution of family-centered care: From supporting parent-delivered interventions to a model of family integrated care. Birth Defects Res 2019;111:1044-59. [Crossref] [PubMed]
- Sabnis A, Fojo S, Nayak SS, et al. Reducing parental trauma and stress in neonatal intensive care: systematic review and meta-analysis of hospital interventions. J Perinatol 2019;39:375-86. [Crossref] [PubMed]
- Meier PP, Engstrom JL, Mingolelli SS, et al. The Rush Mothers' Milk Club: breastfeeding interventions for mothers with very-low-birth-weight infants. J Obstet Gynecol Neonatal Nurs 2004;33:164-74. [Crossref] [PubMed]
- Hurst NM, Myatt A, Schanler RJ. Growth and development of a hospital-based lactation program and mother's own milk bank. J Obstet Gynecol Neonatal Nurs 1998;27:503-10. [Crossref] [PubMed]
- Gharib S, Fletcher M, Tucker R, et al. Effect of Dedicated Lactation Support Services on Breastfeeding Outcomes in Extremely-Low-Birth-Weight Neonates. J Hum Lact 2018;34:728-36. [PubMed]
- Bridges RS. Long-term alterations in neural and endocrine processes induced by motherhood in mammals. Horm Behav 2016;77:193-203. [Crossref] [PubMed]
- Brazelton TB, Tronick E, Adamson L, et al. Early mother-infant reciprocity. Ciba Found Symp 1975;137-54. [PubMed]
- Viaux-Savelon S, Rosenblum O, Guedeney A, et al. Dyssynchrony and perinatal psychopathology impact of child disease on parents-child interactions, the paradigm of Prader Willi syndrom. J Physiol Paris 2016;110:427-33. [Crossref] [PubMed]
- Ionio C, Mascheroni E, Colombo C, et al. Stress and feelings in mothers and fathers in NICU: identifying risk factors for early interventions. Prim Health Care Res Dev 2019;20:e81. [Crossref] [PubMed]
- Lau C, Hurst NM, Smith EO, et al. Ethnic/racial diversity, maternal stress, lactation and very low birthweight infants. J Perinatol 2007;27:399-408. [Crossref] [PubMed]
- Sanders MR, Hall SL. Trauma-informed care in the newborn intensive care unit: promoting safety, security and connectedness. J Perinatol 2018;38:3-10. [Crossref] [PubMed]
- Stotts AL, Villarreal YR, Klawans MR, et al. Psychological Flexibility and Depression in New Mothers of Medically Vulnerable Infants: A Mediational Analysis. Matern Child Health J 2019;23:821-9. [Crossref] [PubMed]
- Riedstra JP, Aubuchon-Endsley NL. A Moderated Mediation Model of Maternal Perinatal Stress, Anxiety, Infant Perceptions and Breastfeeding. Nutrients 2019;11:2981. [Crossref] [PubMed]
- Nath S, Pearson RM, Moran P, et al. Maternal personality traits, antenatal depressive symptoms and the postpartum mother-infant relationship: a prospective observational study. Soc Psychiatry Psychiatr Epidemiol 2020;55:621-34. [Crossref] [PubMed]
- Denis A, Luminet O. Cognitive factors and post-partum depression: What is the influence of general personality traits, rumination, maternal self-esteem, and alexithymia? Clin Psychol Psychother 2018;25:359-67. [Crossref] [PubMed]
- Larsen RJ, Diener E. Affect intensity as an individual difference characteristic: a review. Journal of Research in Personality 1987;21:1-39. [Crossref]
- Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. J Consult Psychol 1960;24:349-54. [Crossref] [PubMed]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6. [Crossref] [PubMed]
- Derogatis LR. Brief Symptom Inventory (BSI). 1975.
- Zimet GD. NW D, SG Z, GK F. The multidimensional scale of perceived social support. J Personality Assessment. 1988;52:30-41. [Crossref]
- Endler NS, Parker JDA. Coping Inventory for Stressful Situations (CISS) Pearson Assessments. 1990.
- Barger SD. The Marlowe-Crowne affair: short forms, psychometric structure, and social desirability. J Pers Assess 2002;79:286-305. [Crossref] [PubMed]
- Dudley NM, McFarland LA, Goodman SA, et al. Racial differences in socially desirable responding in selection contexts: magnitude and consequences. J Pers Assess 2005;85:50-64. [Crossref] [PubMed]
- Marlowe D, Crowne DP. Social desirability and response to perceived situational demands. J Consult Psychol 1961;25:109-15. [Crossref] [PubMed]
- Johnson TP, Fendrick M. A validation of the Crowne-Marlowe social desirability scale. 2002 Proceedings of the Section on Survey Research Methods: Alexandria, VA: American Statistical Association; 2003. p. 1661-6.
- Hynan MT, Hall SL. Psychosocial program standards for NICU parents. J Perinatol 2015;35:S1-4. [Crossref] [PubMed]
- Lau C. Breastfeeding Challenges and the Preterm Mother-Infant Dyad: A Conceptual Model. Breastfeed Med 2018;13:8-17. [Crossref] [PubMed]
- Franck LS, Cox S, Allen A, et al. Measuring neonatal intensive care unit-related parental stress. J Adv Nurs 2005;49:608-15. [Crossref] [PubMed]
- Noergaard B, Ammentorp J, Garne E, et al. Fathers' Stress in a Neonatal Intensive Care Unit. Adv Neonatal Care 2018;18:413-22. [Crossref] [PubMed]
- Abraham E, Hendler T, Shapira-Lichter I, et al. Father's brain is sensitive to childcare experiences. Proc Natl Acad Sci U S A 2014;111:9792-7. [Crossref] [PubMed]
- Prouhet PM, Gregory MR, Russell CL, et al. Fathers' Stress in the Neonatal Intensive Care Unit: A Systematic Review. Adv Neonatal Care 2018;18:105-20. [Crossref] [PubMed]
- Ivashchuk A, Guillen U, Mackley A, et al. Parental protective factors and stress in NICU mothers and fathers. J Perinatol 2020;41:2000-8. [Crossref] [PubMed]
- Beck CT, Vo T. Fathers' stress related to their infants' NICU hospitalization: A mixed research synthesis. Arch Psychiatr Nurs 2020;34:75-84. [Crossref] [PubMed]
Cite this article as: Lau C, Turcich MR, Fraley JK. Mediational models of maternal stress in neonatal intensive care units. Pediatr Med 2022;5:2.

