
Considerations in implementing evidence-based early autism spectrum disorder interventions in community settings
Over the last two decades, research has identified a growing number of efficacious interventions for autism spectrum disorder (ASD) (1,2). There is mounting consensus around the common elements of what works, the ages at which various approaches are appropriate, and the specific ASD symptoms best targeted through psychosocial intervention (3,4). Despite this wealth of knowledge, a concerning gap between research and practice remains: best-practice interventions are not reaching communities where the majority of children and families can benefit from quality care. This gap is particularly evident in early intervention, where best practice guidelines and a wealth of developmental science research support the use of a combination of provider- and parent-implemented naturalistic developmental behavioral interventions (3). Unfortunately, these strategies are rarely utilized effectively in community settings (5,6) Although this problem is broadly generalizable, the pervasive nature of ASD, the intervention complexity, and the intricacies of the service system require unique attention. Careful consideration of the context in which early ASD interventions will be implemented, specifically the fit between interventions and their context, may promote the broader use of evidence-based practices (EBPs) and ultimately benefit a greater number of children and families.
Using an implementation science framework to support community practice
Implementation science is the study of methods to promote the adoption and integration of EBPs and policies into routine care (7). A unidirectional model of developing and testing innovative practices in research settings and then subsequently rolling the practice into communities is rarely successful. Thus, positive intervention effects seen in research labs are not replicated in community practice (8,9). Implementation researchers have developed frameworks that specify the complex context for EBP implementation, and factors that potentially support or hinder the implementation of innovative practices in each stage.
The Exploration, Preparation, Implementation, Sustainment (EPIS) implementation framework has been used to examine ASD services, as it focuses on EBP implementation in publicly funded services targeted to children and families [Figure 1; adapted from Aarons et al. (10)]. The model highlights influential contextual factors within four phases: Exploration, Preparation, Implementation and Sustainment and examines potential barriers or facilitators to the implementation process that may occur in selecting, using, and sustaining an EBP (11).
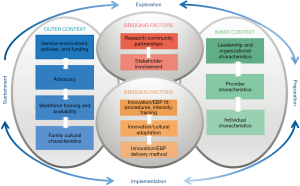
The EPIS model emphasizes the role of context in implementation success. The outer context (e.g., service environment/policies, funding, advocacy), the inner context (e.g., leadership, organizational and provider characteristics), bridging factors (e.g., research-community partnerships), and innovation factors all likely affect implementation. Understanding the influences at each phase allows for a targeted, proactive approach to potential barriers, thus maximizing the successful delivery of an intervention. The EPIS model can serve as a guide for understanding considerations for implementing community-based ASD early interventions.
Below, we discuss several contextual issues relevant for EBP implementation in community early intervention settings serving children with ASD. This discussion is not exhaustive, however, and additional contextual issues likely factor into each phase of implementing any EBP in complex systems.
Outer context
Several outer contextual factors can impact implementation, as follows:
Service environment, policies, and funding
Funding and policies play a large role in determining early intervention for children with ASD in the United States (US) and globally. For example, US children under age 3 with an ASD diagnosis or early signs of ASD are eligible for publicly funded early intervention services. US early intervention services emphasize service provision within the natural environment (often the home), and mandate family inclusion in services. However, states vary greatly in system structure and administration; eligibility criteria; interagency coordination; and service delivery (12,13). Services can range from a monthly visit from a social worker, to intensive interventions involving 20 hours weekly of intervention and parent education.
In other countries, such as Taiwan, services are provided in school settings and may not include parent education (14). Some countries are just beginning to provide publicly funded ASD care and have adopted one specific intervention for all children (15). These policies, of course, affect the intensity and type of services that will be acceptable and feasible in different sites. In reality, most children with ASD in high-income countries do not begin services until about age 5, and children in low- and middle-income counties often do not have access to early intervention at all (16-18). Early engagement of children with ASD in treatment is a strong predictor of future outcomes. Thus, we must increase efforts to develop stronger policies and funding mechanisms to move effective EBPs into these diverse community settings (19).
Advocacy
Community advocacy and parent groups play a significant role in policy and service provision for children with ASD. Perhaps as a reaction to early theories that parents caused ASD, as well as a lack of community treatment options, parent organizations have been instrumental in obtaining the right for children with ASD to attend public schools and in developing a congressional caucus focusing on ASD. Parent organizations that fund research and advocate for evidence-based and alternative treatments have mobilized capital, researchers, and legislators toward changing ASD services (20). Families also influence services individually through legal channels to push service systems to increase service intensity, use specific interventions, and improve provider training (21). In a review of 45 legal cases brought by families against their children’s educational programs, 75% were decided in favor of families (22).
In the US, strong advocacy from parent organizations and providers has led to both public and private insurance funding early intervention for ASD, increasing access to care for many children. However, in some states, regulations have been interpreted as supporting only one EBP. Advocacy on the part of professional organizations has led to the belief that one type of highly structured behavioral intervention exclusively fits the insurance description. This outer context variable interacts with inner and intervention context variables. For example, highly structured treatments are often easier to implement for community agencies training paraprofessionals to work with limited supervision, thus making this interpretation helpful (23). This level of structure, however, is a specific challenge for early interventionists, as the high level of structure does not fit a developmental model, nor is it consistent with current best practice recommendations or policies that support naturalistic interventions (3). Consequently, this type of advocacy and interpretation of the regulations can affect services in specific areas.
Workforce availability
Another important outer context variable related to the service environment is workforce availability. In general, early intervention is more available in larger urban areas in the US, and high-income countries globally, due to access to highly educated specialists with training in EBPs. One response to limited access to professionals with ASD experience and cost-effective interventions has been to adopt parent-implemented approaches. These interventions, which target challenging child behaviors, parent-child interactions, and child social communication skills, have produced promising, sustained improvements in child developmental and behavioral outcomes, including low-intensity programs (24-26). Other approaches have addressed workforce training and cost issues through use of non-specialists to deliver EBPs for young children with ASD (27). These efforts have implications for other contextual variables including specialist training, cultural issues, and family engagement.
Family cultural characteristics
In spite of well-documented socioeconomic disparities in ASD diagnoses and service use, the field has essentially overlooked the diverse sociocultural contexts in which children live (28-30). Most ASD intervention studies have been conducted primarily with White, upper/middle-class families (31,32). The scarcity of early intervention studies inclusive of low-income families is particularly concerning in light of the additional financial stressors they face, as high service cost can limit care options (33). Low-income communities often lack experienced healthcare providers to provide parents with appropriate referrals, even when parents proactively seek out this information (34). Thus, children living with less well-educated caregivers or in low-income neighborhoods are frequently diagnosed with ASD later than their more affluent peers, oftentimes after they enter the school system and beyond the age to take advantage of early intervention (35,36). In response, some researchers have adapted early interventions for children in low-income families, although limited community engagement impacted participation (37,38).
Enrolling families from diverse racial and ethnic groups in research and intervention may be a challenge (39). In general, barriers within the ASD service system are more substantial for low-income and ethnic minority families (40,41). In the US, delayed ASD diagnoses and limited contact with early intervention for both Latinx and Black children are particularly significant. Compared to White children, Black children were less likely to receive a developmental evaluation before age 3, or access early intervention (16,42). Similarly, children of Latinx parents for whom English was not their primary language in particular experience delayed access to care (43). Furthermore, Latinx and Black caregivers of children with ASD report mistrust of their child’s providers, fewer therapy hours, perceived provider racial bias, and poor caregiver-provider interactions (40,44-47).
Other cultural factors can influence timely ASD intervention and treatment engagement, including autism stigma (45,48). In turn, stigma is associated with a negative impact on family life (49). In total, these factors suggest careful attention to the myriad of family- and community-related factors impacting early intervention options for children with ASD.
Inner context
Inner contextual factors focus on organizational elements impacting implementation. Below, we discuss three factors relevant to ASD early interventions.
Leadership and organizational characteristics
Traditionally, EBP training focuses on providers’ role in learning and using the intervention. However, recent research highlights the importance of leadership in successful implementation of innovative practices (50-53). Researchers have identified specific behaviors and actions that demonstrate a leader’s commitment to, knowledge of, support for, and perseverance during EBP implementation (54). Supports such as professional trainings, access to resources, and ongoing performance monitoring have been linked to better sustainment of an intervention, improved child outcomes, and decreased staff burnout and turnover (55). ASD intervention studies specifically have identified a clear relationship between these organizational factors and child-level outcomes (56-58). It is critical we consider the role of the leadership and organizational support for both training and ongoing EBP use when implementing interventions in new communities.
Provider characteristics
Provider characteristics are crucial to treatment implementation. For example, knowledge about ASD and ASD EBPs are associated with later treatment fidelity (59). Additionally, provider attitudes towards EBPs predict use and sustainment of new interventions. For example, US early intervention providers generally expect to work directly with children with broad developmental delays. They typically do not have the expectation or education to coach parents effectively, nor to address ASD symptoms specifically (60). Although the early intervention field has begun to focus on how to optimally coach parents, as well as how to address ASD-related symptoms (61-63), we need to alter provider expectations and preparation for their roles in order to support successful implementation.
Individual characteristics
Intervention goals and strategies should be individualized based on the child’s developmental needs, in combination with the family’s priorities. Many evidence-based early interventions do this by using careful assessments, family collaboration, and comprehensive provider training (64). Researchers are just beginning to understand how to individualize strategies based on a priori child characteristics (65,66). This information needs to be translated into methods feasible for providers in order to be widely implemented.
The focus on parent-implemented intervention in ASD early intervention presents additional individualization challenges. Caregiver coordination of ASD services can place significant demands on families, and consideration of family characteristics during the ASD treatment planning process can improve early intervention initiation and retention (67,68). Although most studies find parent education and training reduces parental stress and increases family empowerment, a subset of parents (perhaps up to one-third) may not benefit from parent training if they have extremely high levels of stress (69-71). Therefore, parent involvement needs to be individualized based on the child and family’s needs and capacities at the time of intervention. For example, play-based approaches which complement existing child-focused early interventions and address parenting stress can provide parents with developmentally appropriate, less structured methods to support their children (72).
Innovation (EBP) factors
Given the outer contextual challenges, and the fact that most ASD EBPs were developed under controlled research conditions, EBP developers need to be flexible in shaping their interventions for implementation in community contexts. Moreover, particular attention must be paid to ongoing evaluation, in order to detect changes in effectiveness in a particular setting. There have been some attempts to increase the fit of an EBP with the intervention context (e.g., schools or community mental health clinics) by adapting specific procedures, intensity and training strategies, which have led to improved feasibility, acceptability and training outcomes in these contexts (73-75). For example, group-based ASD parent training models offer community agencies opportunities to simultaneously intervene with multiple families of young children, build peer social support, and reduce program costs (76-78).
Some researchers have begun to develop culturally relevant ASD interventions to meet the needs of diverse communities in the US, including Black and Latinx children with ASD, as racial and ethnic disparities persist even after controlling for socioeconomic differences (29,31,79). The majority of US studies have investigated service disparities between Black, Latinx, and White children and their families, although emerging research has identified barriers for Asian immigrant communities as well (80,81). Globally, researchers have culturally adapted EBPs, for example using a task-shifting approach in South Asia, and a combined parent-teacher training model for refugee families in Turkey (27,82). In total, these studies point to the need for more interventions designed to meet the needs of culturally diverse communities, as well a wider array of intervention delivery methods (e.g., online or group-based).
Bridging factors
One approach to tackle the complex challenges of implementing EBPs in community early intervention is to bring stakeholders together in a research-community partnership. Stakeholder involvement can address potential ideological differences; and increased communication between researchers and community partners can ensure community EBP implementation with higher levels of acceptability, feasibility, and utility.
One example of this type of partnership in the context of early ASD intervention is the Southern California BRIDGE Collaborative [as described in Brookman-Frazee et al. (75)]. BRIDGE is a community-academic partnership developed to improve interventions for young children with or at-risk for ASD and their families. The Collaborative consists of clinicians, funding agency representatives, parents, and researchers with expertise in ASD and/or the intervention service system. Early in the development of the Collaborative (which began meeting in 2007), members jointly decided to target the implementation of evidence-based, parent-implemented practices in community settings as their primary purpose. Over the last 12 years, members have worked together to utilize specific implementation strategies (53,83) and address barriers in the outer and inner contexts in order to build community capacity to serve toddlers with ASD and their families. These strategies have targeted every phase of implementation (i.e., Exploration, Preparation, Implementation and Sustainment), with particular attention to many of the issues discussed here (e.g., individualizing service based on family need, effective provider training) (84). Indeed, the involvement of a community-academic partnership in and of itself is an implementation strategy that can improve EBP use in multiple settings (53,83,85).
The result of the Collaborative’s work across the last decade is the broad local community implementation of a particular EBP that the Collaborative specifically adapted for use with toddlers with social communication concerns. Pilot testing found significantly greater improvements in positive parent-child interactions with the adapted intervention than in usual community care. Because funding agency representatives participated in the Collaborative to select the particular EBP, the adapted intervention is currently publicly funded for children at risk for ASD under age three, resulting in increased agencies requesting training and greater capacity and family access to services. Additionally, agencies who typically deliver highly structured interventions are now motivated to learn these more developmentally appropriate strategies, due to their tie to public funding. Overall, the Collaborative has been highly successful in deploying a particular EBP in the community due to the shared input from all stakeholders.
Conclusions and recommendations
Early intervention is a critical component to any ASD service system. Despite the increasing prevalence of ASD, many children do not receive early intervention due to delayed diagnoses and various other factors. Community-based ASD early interventions can better identify children and provide interventions in more naturalistic environments for young children and their families. In this article, we have discussed several barriers and potential opportunities facing the dissemination and uptake of community-based early ASD interventions. Using the EPIS framework, we explored how both outer and inner contextual factors, along with the EBPs themselves, can work together to either impede or facilitate effective implementation within communities. We provided an example of a successful bridging factor, which harnessed the efforts and expertise of families, funding agencies, researchers, clinicians, and other stakeholders to address the common goal of improving the outcomes of young children with ASD and their families. We hope this framework will assist researchers in moving EBP into community early intervention settings successfully.
Acknowledgments
The authors would like to thank the many researcher and community-based collaborators who have helped to shape this work. Providers and families in many settings have generously provided input and participation to help understand the complexities of improving community early intervention programs. We appreciate Nicole Garbarino for her help to format the article.
Funding: The community partnership described in this paper was supported in part by the U.S. Department of Education (R324A140004), Autism Speaks [8136] and the AC Stahmer received infrastructure support through the MIND Institute IDDRC funded by the National Institute of Child Health and Human Development (U54 HD079125).
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Geraldine Dawson and Lauren Franz) for the series “Implementing Autism Early Intervention” published in Pediatric Medicine. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/pm.2019.05.01). The Series “Implementing Autism Early Intervention” was commissioned by the editorial office without any funding or sponsorship. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- The National Autism Center. National Standards Project Findings and Conclusions. Randolph, Massachusetts, 2009.
- The National Autism Center. Findings and Conclusions: National Standards Project, Phase 2. Randolph, Massachusetts, 2015.
- Schreibman L, Dawson G, Stahmer AC, et al. Naturalistic developmental behavioral interventions: empirically validated treatments for autism spectrum disorder. J Autism Dev Disord 2015;45:2411-28. [Crossref] [PubMed]
- Wong C, Odom SL, Hume K, et al. Evidence-based practices for children, youth, and young adults with autism spectrum disorder. Chapel Hill: The University of North Carolina, Frank Porter Graham Child Development Institute, Autism Evidence-Based Practice Review Group, 2014.
- Coogle CG, Guerette AR, Hanline MF. Early intervention experiences of families of children with an autism spectrum disorder: a qualitative pilot study. Early Childhood Research & Practice 2013;15:
- Hume K, Bellini S, Pratt C. The Usage and perceived outcomes of early intervention and early childhood programs for young children with autism spectrum disorder. Topics Early Child Spec Educ 2005;25:195-207. [Crossref]
- Eccles MP, Mittman BS. Welcome to implementation science. Implement Sci 2006;1:1. [Crossref]
- Glasgow RE, Lichtenstein E, Marcus AC. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health 2003;93:1261-7. [Crossref] [PubMed]
- Lenfant C. Shattuck lecture--clinical research to clinical practice--lost in translation? N Engl J Med 2003;349:868-74. [Crossref] [PubMed]
- Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health 2011;38:4-23. [Crossref] [PubMed]
- Walsh C, Rolls Reutz J, Williams R. Selecting and implementing evidence-based practices: a guide for child and family serving systems. 2nd edition. San Diego, CA: California Evidence-Based Clearinghouse for Child Welfare, 2015.
- Danaher J, Shackelford J, Harbin G. Revisiting a comparison of eligibility policies for infant/toddler programs and preschool special education programs. Topics Early Child Spec Educ 2004;24:59-67. [Crossref]
- Fitzgerald HE, Freeark-Zucker K, Zucker R. The crisis in youth mental health: critical issues and effective programs. 1st edition. Westport, CT: Praeger, 2006:109-131.
- Lee LC, Stahmer AC, Wu CC, et al. Home-based, parent-implemented intervention for underserved families in Taiwan. In: Siller M, Morgan L. editors. Handbook of family-centered practice for very young children with autism. New York, NY: Springer, 2018:385-391.
- Taha GRA, Hussein H. Autism spectrum disorders in developing countries: lessons from the Arab world. In: Patel V, Preedy V, Martin C. editors. Comprehensive guide to autism. New York, NY: Springer, 2014.
- Christensen DL, Baio J, Van Naarden Braun K, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years--Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2012. MMWR Surveill Summ 2016;65:1-23. [Crossref] [PubMed]
- Devescovi R, Monasta L, Mancini A, et al. Early diagnosis and Early Start Denver Model intervention in autism spectrum disorders delivered in an Italian public health system service. Neuropsychiatr Dis Treat 2016;12:1379-84. [Crossref] [PubMed]
- Divan G. Editorial Perspective: 'From there to here': adapting child and adolescent mental health interventions for low-resource settings. J Child Psychol Psychiatry 2017;58:325-7. [Crossref] [PubMed]
- Croen LA, Shankute N, Davignon M, et al. Demographic and clinical characteristics associated with engagement in behavioral health treatment among children with autism spectrum disorders. J Autism Dev Disord 2017;47:3347-57. [Crossref] [PubMed]
- Metz B, Mulick JA, Butter EM. Autism: A late-20th-century fad magnet. In: Jacobson JW, Foxx RM, Mulick JA. editors. Controversial therapies for developmental disabilities: Fad, fashion and science in professional practice. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers, 2005:237-63.
- Jacobson JW. Early intensive behavioral intervention: emergence of a consumer-driven service model. Behav Anal 2000;23:149-71. [Crossref] [PubMed]
- Yell ML, Drasgow E. Litigating a free appropriate public education: the Lovaas hearings and cases. J Spec Educ 2000;33:205-14. [Crossref]
- Stahmer AC, Reed S, Lee E, et al. Training teachers to use evidence-based practices for autism: examining procedural implementation fidelity. Psychol Sch 2015;52:181-95. [Crossref] [PubMed]
- Bearss K, Johnson C, Smith T, et al. Effect of parent training vs parent education on behavioral problems in children with autism spectrum disorder: a randomized clinical trial. JAMA 2015;313:1524-33. [Crossref] [PubMed]
- Kasari C, Paparella T, Freeman S, et al. Language outcome in autism: randomized comparison of joint attention and play interventions. J Consult Clin Psychol 2008;76:125-37. [Crossref] [PubMed]
- Reichow B, Servili C, Yasamy MT, et al. Non-specialist psychosocial interventions for children and adolescents with intellectual disability or lower-functioning autism spectrum disorders: a systematic review. PLoS Med 2013;10:e1001572; discussion e1001572.
- Divan G, Hamdani SU, Vajartkar V, et al. Adapting an evidence-based intervention for autism spectrum disorder for scaling up in resource-constrained settings: the development of the PASS intervention in South Asia. Glob Health Action 2015;8:27278. [Crossref] [PubMed]
- Daniels AM, Mandell DS. Explaining differences in age at autism spectrum disorder diagnosis: a critical review. Autism 2014;18:583-97. [Crossref] [PubMed]
- Durkin MS, Maenner MJ, Baio J, et al. Autism spectrum disorder among US children (2002-2010): socioeconomic, racial, and ethnic disparities. Am J Public Health 2017;107:1818-26. [Crossref] [PubMed]
- Nguyen CT, Krakowiak P, Hansen R, et al. Sociodemographic disparities in intervention service utilization in families of children with autism spectrum disorder. J Autism Dev Disord 2016;46:3729-38. [Crossref] [PubMed]
- Jamison JM, Fourie E, Siper PM, et al. Examining the efficacy of a family peer advocate model for black and Hispanic caregivers of children with autism spectrum disorder. J Autism Dev Disord 2017;47:1314-22. [Crossref] [PubMed]
- Lord C, Wagner A, Rogers S, et al. Challenges in evaluating psychosocial interventions for autistic spectrum disorders. J Autism Dev Disord 2005;35:695-708; discussion 709-11. [Crossref] [PubMed]
- Flanders SC, Engelhart L, Pandina GJ, et al. Direct health care costs for children with pervasive developmental disorders: 1996-2002. Adm Policy Ment Health 2007;34:213-20. [Crossref] [PubMed]
- Ruble LA, Heflinger CA, Renfrew JW, et al. Access and service use by children with autism spectrum disorders in Medicaid managed care. J Autism Dev Disord 2005;35:3-13. [Crossref] [PubMed]
- Dickerson AS, Rahbar MH, Pearson DA, et al. Autism spectrum disorder reporting in lower socioeconomic neighborhoods. Autism 2017;21:470-80. [Crossref] [PubMed]
- Palmer RF, Blanchard S, Jean CR, et al. School district resources and identification of children with autistic disorder. Am J Public Health 2005;95:125-30. [Crossref] [PubMed]
- Carr T, Shih W, Lawton K, et al. The relationship between treatment attendance, adherence, and outcome in a caregiver-mediated intervention for low-resourced families of young children with autism spectrum disorder. Autism 2016;20:643-52. [Crossref] [PubMed]
- Carr T, Lord C. A pilot study promoting participation of families with limited resources in early autism intervention. Res Autism Spectr Disord 2016;2:87-96. [Crossref] [PubMed]
- Shaia WE, Nichols HM, Dababnah S, et al. Brief report: participation of black and African-American families in autism research. J Autism Dev Disord 2019; [Epub ahead of print]. [Crossref] [PubMed]
- Zuckerman KE, Lindly OJ, Sinche BK. Parental concerns, provider response, and timeliness of autism spectrum disorder diagnosis. J Pediatr 2015;166:1431-9.e1. [Crossref] [PubMed]
- Magaña S, Parish SL, Rose RA, et al. Racial and ethnic disparities in quality of health care among children with autism and other developmental disabilities. Intellect Dev Disabil 2012;50:287-99. [Crossref] [PubMed]
- Feinberg E, Silverstein M, Donahue S, et al. The impact of race on participation in part C early intervention services. J Dev Behav Pediatr 2011;32:284-91. [Crossref] [PubMed]
- St Amant HG, Schrager SM, Peña-Ricardo C, et al. Language barriers impact access to services for children with autism spectrum disorders. J Autism Dev Disord 2018;48:333-40. [Crossref] [PubMed]
- Angell AM, Solomon O. The social life of health records: understanding families’ experiences of autism. Soc Sci Med 2014;117:50-7. [Crossref] [PubMed]
- Dababnah S, Shaia WE, Campion K, et al. “We Had to Keep Pushing”: caregivers’ perspectives on autism screening and referral practices of black children in primary care. Intellect Dev Disabil 2018;56:321-36. [Crossref] [PubMed]
- Magaña S, Parish SL, Son E. Have racial and ethnic disparities in the quality of health care relationships changed for children with developmental disabilities and ASD? Am J Intellect Dev Disabil 2015;120:504-13. [Crossref] [PubMed]
- Pearson J, Meadan H. African American parents’ perceptions of diagnosis and services for children with autism. Educ Train Autism Dev Disabil 2018;53:17-32.
- Burkett K, Morris E, Manning-Courtney P, et al. African American families on autism diagnosis and treatment: the influence of culture. J Autism Dev Disord 2015;45:3244-54. [Crossref] [PubMed]
- Kinnear SH, Link BG, Ballan MS, et al. Understanding the experience of stigma for parents of children with autism spectrum disorder and the role stigma plays in families’ lives. J Autism Dev Disord 2016;46:942-53. [Crossref] [PubMed]
- Bass BM, Avolio BJ. The implications of transformational and transactional leadership for individual, team, and organizational development. In: Woodman RW, Pasmore W. editors. Research in Organizational Change and Development. Greenwich, CT: JAI Press, 1990:231-72.
- Stogdill RM. Handbook of Leadership: A Survey of Theory and Research. New York, NY: The Free Press, 1974.
- Edmondson AC. Speaking up in the operating room: how team leaders promote learning in interdisciplinary Action Teams. J Manag Stud 2003;40:1419-52. [Crossref]
- Powell BJ, McMillen JC, Proctor EK, et al. A compilation of strategies for implementing clinical innovations in health and mental health. Med Care Res Rev 2012;69:123-57. [Crossref] [PubMed]
- Aarons GA, Green AE, Trott E, et al. The roles of system and organizational leadership in system-wide evidence-based intervention sustainment: a mixed-method study. Adm Policy Ment Health 2016;43:991-1008. [Crossref] [PubMed]
- Novins DK, Green AE, Legha RK, et al. Dissemination and implementation of evidence-based practices for child and adolescent mental health: a systematic review. J Am Acad Child Adolesc Psychiatry 2013;52:1009-1025.e18. [Crossref] [PubMed]
- Glisson C, Hemmelgarn A, Green P, et al. Randomized trial of the Availability, Responsiveness and Continuity (ARC) organizational intervention for improving youth outcomes in community mental health programs. J Am Acad Child Adolesc Psychiatry 2013;52:493-500. [Crossref] [PubMed]
- Williams NJ, Glisson C. Testing a theory of organizational culture, climate and youth outcomes in child welfare systems: a United States national study. Child Abuse Negl 2014;38:757-67. [Crossref] [PubMed]
- Dingfelder HE, Mandell DS. Bridging the research-to-practice gap in autism intervention: an application of diffusion of innovation theory. J Autism Dev Disord 2011;41:597-609. [Crossref] [PubMed]
- Suhrheinrich J, Rieth SR, Dickson KS, et al. Classroom pivotal response teaching: teacher training outcomes of a community efficacy trial. Teach Educ Spec Educ 2019; [Epub ahead of print].
- Fleming JL, Sawyer LB, Campbell PH. Early intervention providers’ perspectives about implementing participation-based practices. Topics Early Child Spec Educ 2010;30:233-44. [Crossref]
- Fettig A, Barton EE. Parent implementation of function-based intervention to reduce children’s challenging behavior: a literature review. Topics Early Child Spec Educ 2013;34:49-61. [Crossref]
- Friedman M, Woods J, Salisbury C. Caregiver coaching strategies for early intervention providers: moving toward operational definitions. Infants & Young Children 2012;25:62-82. [Crossref]
- Stahmer AC, Brookman-Frazee L, Rieth SR, et al. Parent perceptions of an adapted evidence-based practice for toddlers with autism in a community setting. Autism 2017;21:217-30. [Crossref] [PubMed]
- Ingersoll B, Dvortcsak A. Teaching social communication to children with autism: a practitioner’s guide to parent training. In: Teaching Social Communication to Children with Autism: A Practitioner’s Guide to Parent Training. New York, NY: The Guilford Press, 2010.
- Sherer MR, Schreibman L. Individual behavioral profiles and predictors of treatment effectiveness for children with autism. J Consult Clin Psychol 2005;73:525-38. [Crossref] [PubMed]
- Yoder P, Stone WL. A randomized comparison of the effect of two prelinguistic communication interventions on the acquisition of spoken communication in preschoolers with ASD. J Speech Lang Hear Res 2006;49:698-711. [Crossref] [PubMed]
- Karst JS, Van Hecke AV. Parent and family impact of autism spectrum disorders: a review and proposed model for intervention evaluation. Clin Child Fam Psychol Rev 2012;15:247-77. [Crossref] [PubMed]
- Stahmer AC, Schreibman L, Cunningham AB. Toward a technology of treatment individualization for young children with autism spectrum disorders. Brain Res 2011;1380:229-39. [Crossref] [PubMed]
- Robbins FR, Dunlap G, Plienis AJ. Family characteristics, family training, and the progress of young children with autism. J Early Interv 1991;15:173-84. [Crossref]
- Singer GH, Goldberg-Hamblin SE, Peckham-Hardin KD, et al. Toward a synthesis of family support practices and positive behavior support. In: Lucyshyn JM, Dunlap G, Albin RW. editors. Family, community & disability. Families and positive behavior support: Addressing problem behavior in family contexts. Baltimore, MD, US: Paul H Brookes Publishing, 2002:155-83.
- Webster-Stratton C, Reid MJ. The incredible years parents, teachers and children training series: A multifaceted treatment approach for young children with conduct problems. In: Kazdin AE, Weisz JR. editors. Evidence-based psychotherapies for children and adolescents. New York, NY, US: The Guilford Press, 2003:224-40.
- Dababnah S, Olson EM, Nichols HM. Feasibility of the Incredible Years Parent Program for preschool children on the autism spectrum in two U.S. sites. Res Autism Spectr Disord 2019;57:120-31. [Crossref]
- Stahmer AC, Suhrheinrich J, Reed S, et al. What works for you? Using teacher feedback to inform adaptations of pivotal response training for classroom use. Autism Res Treat 2012;2012:709861 [Crossref] [PubMed]
- Stahmer AC, Suhrheinrich J, Rieth S. A Pilot Examination of the adapted protocol for classroom pivotal response teaching. J Am Acad Spec Educ Prof 2016 Winter:119-39.
- Brookman-Frazee LI, Drahota A, Stadnick N. Training community mental health therapists to deliver a package of evidence-based practice strategies for school-age children with autism spectrum disorders: a pilot study. J Autism Dev Disord 2012;42:1651-61. [Crossref] [PubMed]
- Webster-Stratton C, Dababnah S, Olson E. The Incredible Years® Group-Based Parenting Program for Young Children with Autism Spectrum Disorder. In: Siller M, Morgan L. editors. Handbook of Parent-Implemented Interventions for Very Young Children with Autism. New York: Springer International Publishing, 2018:261-82.
- Dababnah S, Parish SL. Feasibility of an empirically based program for parents of preschoolers with autism spectrum disorder. Autism 2016;20:85-95. [Crossref] [PubMed]
- Tudor Edwards R, Jones C, Berry V, et al. Incredible Years Parenting Programme: cost-effectiveness and implementation. J Child Serv 2016;11:54-72. [Crossref]
- Magaña S, Lopez K, Machalicek W. Parents taking action: a psycho-educational intervention for Latino parents of children with autism spectrum disorder. Fam Process 2017;56:59-74. [Crossref] [PubMed]
- Singh JS, Bunyak G. Autism disparities: a systematic review and meta-ethnography of qualitative research. Qual Health Res 2019;29:796-808. [Crossref] [PubMed]
- Wang H, West EA. Asian American immigrant parents supporting children with autism: perceptions of fathers and mothers. International Journal of Whole Schooling 2016;12:1-21.
- Dababnah S, Habayeb S, Bear BJ, et al. Feasibility of a trauma-informed parent–teacher cooperative training program for Syrian refugee children with autism. Autism. 2018; [Crossref] [PubMed]
- Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci 2015;10:21. [Crossref] [PubMed]
- Rieth SR, Haine-Schlagel R, Burgeson M, et al. Integrating a parent-implemented blend of developmental and behavioral intervention strategies into speech-language treatment for toddlers at risk for autism spectrum disorder. Semin Speech Lang 2018;39:114-24. [Crossref] [PubMed]
- Drahota A, Meza RD, Brikho B, et al. Community-academic partnerships: a systematic review of the state of the literature and recommendations for future research. Milbank Q 2016;94:163-214. [Crossref] [PubMed]
Cite this article as: Stahmer AC, Dababnah S, Rieth SR. Considerations in implementing evidence-based early autism spectrum disorder interventions in community settings. Pediatr Med 2019;2:18.

