Narrative review of therapeutical options in pectus carinatum in young patients
Introduction
Pectus carinatum is the most frequent protrusion deformity of the chest wall (1) but includes less than 10% of chest wall defects. It occurs mostly in young males with a male/female ratio of 4:1 and it has a prevalence of 0.6% (2).
The pathology is usually due to the overgrowth of the costal cartilages (usually 3–7 ribs) and the anterior displacement of the sternum. An increased family incidence suggests a familiar basis of the condition however the pathogenesis is chiefly unknown (3). PC can be associated to the Marfan’s syndrome (4), scoliosis and other deformities of the spine. The deformity is rarely present at birth and often progress during early childhood especially at puberty, that is why the malformation is not identified until after the 11th birthday.
The condition can be divided in four categories, depending on type of the defect:
- Chondrogladiolar: it is the most frequent condition consisting of anterior protrusion of the body of the sternum associated to a lateral depression of the costal cartilages (Figure 1).
- Chondromanubrial: it is the less common deformity and consist of the protrusion of the upper part of the sternum involving the manubrium and the second and third costal cartilages, associated to the depression of the inferior part of the sternum. This condition is also called “pouter pigeon” or “pigeon chest” and can be associated to congenital heart defect (5).
- Asymmetric: consisting of the anterior displacement of the costal cartilages on one side and normal cartilages on the contralateral side (Figure 2).
- Meld: it consists of a carinate deformity on one side and an excavatum deformity on the contralateral side, often causing a sternal rotation. Some authors classify these as a variant of the excavatum deformities.
In 1987, Haller et al. (6) proposed an index based on the images on CT scan to objectify the severity of the malformation, this index is calculated dividing the width of the chest by the distance between the sternum and spine. The index for both young and elder people with a normal chest is 2.54 while for PC patients the severity index range from 1.7 to 2.1 (7).
This condition is not very often connected to severe physical illness, nevertheless, due to the fact that the malformation is difficult to hide, patients prefer the deformity to be corrected. As a matter of fact, this physical state cause ad alteration in the perceived body image and its correction can improve mental health and self-esteem of the patients (8-10). The treatment of PC can be performed either through non-invasive methods (brace) or surgical ones, the latter earmarked for the severe cases and the non-responder at the conservative methods.
Aim of this article is to describe the current state of art.
Methods
We reviewed the literature and analysed the articles through PubMed searching the words “pectus carinatum” “surgical treatment” “PC childhood” “brace”. We also research reviews and items in the Cochrane Library.
Non-surgical techniques
Observation
Pectus carinatum can be diagnosed in infants and children younger than 10 years. In most cases, the wall defect is mild-moderate and remains stable during the first decade of life. It can start to increase or become socially symptomatic at the beginning of adolescence. Therefore, treatment during the first decade of life is rarely indicated. How much the pectus carinatum distorts the body image is a very personal aspect and varies from case to case and the patient’s motivation is extremely important for any active treatment of the PC. In some cases, when the patient does not suffer in an insignificant manner and the motivation for surgical treatment is not high, observation over time is indicated. In these cases, Emil et al. (8) prescribe a posture and a muscle strengthening program of the chest wall. Increasing the muscle mass of the chest wall can improve the general appearance of some patients, but there is no evidence that the exercise alone can correct bone or cartilage deformity.
Bracing
Evidence supporting the use of bracing for pectus carinatum has existed since 1977 (11). Subsequently, Haje and Bowen, both orthopedic surgeons, published their bracing experience in 1992 (12). Then, a study by Canadian pediatric surgeons showed how this technique is used in a widely manner and how it passed the surgical procedures as an initial treatment in selected patients (2). So, in the last ten years, bracing has gained considerable popularity.
There are many bracing devices, but certainly the most revolutionary was invented by Martinez-Ferro et al. (13): in fact, they have developed a dynamic compression system (DCS) that allows measurement of the pressure necessary for initial correction. They have considered the chest wall compliance, related to a primary factor: the age. Then they have found that older children required more pressure and duration of treatment to achieve a satisfactory correction. This system allows you to measure chest wall pressure, in pounds per square inch (psi). During the first evaluation the correction pressure allows the stratification of patients into categories based on the stiffness of the chest wall. It is also possible to set a treatment pressure, which can be varied over time, in order to optimize the compression of the pectus, while maintaining patient comfort. This DCS tutor has led to success rates of over 70% reported in published studies (13-18).
The bracing protocol is based to apply long-term continuous pressure at the deformity protrusion to allow costal cartilage remodeling. Pectus carinatum corrective bracings surround the thorax and have two points of contact: an anterior point which provides direct pressure to the deformity and a second point which determines a back pressure, typically at the patient’s back. For best results, the chest wall must be “malleable”, typically present in the pre-adolescent patient (13,19-21). As such, children aged 10 to 15 years are the best candidates for this technique.
In our experience brace is ideal for patients who have the chondrogladiolar malformation due to the position where the device acts while it has no indication in pigeon chest. These patients cannot benefit from this equipment.
The current literature shows an extreme variety in the protocols implemented in the different centers that use this technique. The duration of bracing is recommended to continue until the result is satisfactory for the patient, for a defined period of 6 months (12) or until the complete growth (19,20). The recommended time for wearing the brace changes in literature from 14 (20) to 24 h per day (21). Other protocols recommend the use of the brace 23 hours a day until the deformity is resolved, followed by a maintenance phase that lasts until the growth is completed, during which the patient wears the brace only during the night (19). However, it has been seen that the most common cause of bracing failure is patient compliance. Wearing a brace for a prolonged period is not a simple thing for a teenager (comfort, clothing, discomfort with peers, up to bullying).
Emil et al. (18) reported the results of a 4-year prospective study of the DCS, who specifically sought to identify the predictors of success. They examined four factors to evaluate patients with PC: sex, age, symmetry and correction pressure. They founded that asymmetry and old age were associated with a higher failure rate. Age is a fundamental factor, as it is inversely proportional to the daily duration of bracing: a longer active treatment period, as we say before, is required in older patients. The correction pressure did not show a correlation between the duration of treatment and the success rate. So far there is no correction pressure value which constitutes a contraindication to bracing. Moreover, in the same study, it is highlighted how the advanced age and the asymmetry of the thorax are not absolute contraindications to the treatment.
Instead, Pessanha et al. (22), founded another fundamental fact: the patients were more easily not complying with the duration rather than the frequency of the use of the brace: they wore the brace every day, but for shorter period. Kang et al. (23) discovered that the most important predictor of compliance was the evidence of a good result during the first 2 or 4 weeks.
However, we have to consider that, the long-term effectiveness of this treatment modality is unknown. Martinez-Ferro et al. (13) found a recurrence rate of 15% at a mean follow-up of 3.3 years, but they observed that all relapses achieved full resolution with further bracing treatment.
Complications with bracing are minor, especially when we compare it with invasive surgical treatments: rash or skin discoloration or cutaneous ulceration at the point of brace’s contact, back pain and hematoma have been reported (13) reported 15 cases of overcorrection that lead to having an iatrogenic pectus excavatum. Frequent follow-up is therefore important to ensure appropriate adaptation and correction.
Therefore, as stated by Desmarais et al. (24), bracing should be presented to patients as an effective non-surgical therapy, which avoids the risks associated with surgery, while still allowing surgery at a later date, if it is necessary (17). Patient’s compliance remains the only necessary characteristic. In fact, lack of motivation is perhaps the only real contraindication to bracing.
Surgical technique
One of the first author who proposed a surgical treatment for PC has been Dr MM Ravitch in 1952. He described the surgical treatment of PC in a young boy with pouter pigeon breast symptomatic for tachycardia. He performed the resection of portions of five costal cartilages on both sides, then proceeded with a cuneiform osteotomy at the manubriosternal junction to allow the corpus sterni to be elevated forward and a second osteotomy in the reverse direction in the medial part of the sternum. This consented the distal portion of the sternum to be flexed posteriorly, correcting the concavity. The aim of the procedure was to reduce the lateral depressions and relieve the possible compression of the heart (25). In 1960, he published a new article in which he described a new approach for PC in an 18 years old boy with a cavity on both side of the sternum that was unusually prominent. The operation was done in two different steps. The first procedure was on the right side; the incision was made in the midline of the sternum and then across to the right axillary line, through the deepest point of the lateral concavity. The thoracic cage was completely exposed by the reflection of the pectoralis major and the rectus abdominis. The most prominent parts of the costal cartilages were cut and the cartilages most deeply depressed were resected subperichondrially for the entire length of the depressed portion. This allowed the concavity to be corrected. The new state was maintained thanks to a reefing suture in the perichondrium. The same kind of surgery was performed on the other side 8 months later (26).
This technique has been largely widespread and during years has evolved. Robicsek in 1963 suggested another method of surgery which consist in creating an upper sternal osteotomy and resecting the lower angulated portion with the sternum and the xyphoid (27).
The mid-long-term results have been encouraging and the technique has remained approximately the same for many years with only little variations depending on the team performing surgery.
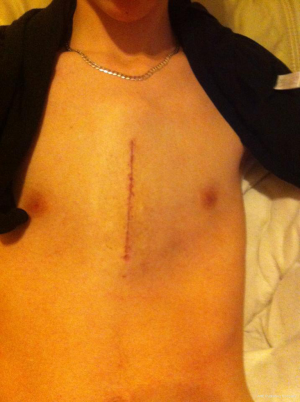
Scarci et al. proposed the surgical treatment for those patients who have low compliance with the brace or moderate to severe asymmetry (Figure 3) (28).
Even in our centre, we prefer to treat young patient with brace and set aside surgery only in case of severe malformation. In these cases, we performed an open procedure with the resection of 3–4 costal cartilages and a sternal osteotomy.
All these procedures require a large skin incision, sternal osteotomies, the resection of the costal cartilage and sometimes muscle flap. The long term-outcome can include pain, dysesthesia, pneumothorax, bleeding, seroma formation, scars and keloid in patients who are usually young and with self-esteem problems (29).
Nowadays several minimally invasive techniques have been proposed (30).
Kobayashi et al. in 1997 treated the PC exploiting the endoscopic visualization: he performed the partial resection of the 3rd or 4th to 8th costal cartilages and a wedge-osteotomy of the sternum at the point of maximum curvature with a small skin incision in the pre xyphoid region (31).
The new approach proposed by Nuss for the treatment of pectus excavatum, which consist in the possibility of manage the malformation without the resection of the costal cartilages, using the placement of a metal bar, leaded the way for new and less invasive procedures. In 2005, Abramson et al. suggested an alternative to open surgery in selected patients with a good elasticity of the chest wall. In these cases, an intrathoracic compression is performed implanting a metal bar in the presternal region and securing it to both side to the posterolateral portion of the costal arches. The bar remains implanted until the outline of the shape is the one wished depending on the growth of the single patient (32). This technique requires only two small incisions in the lateral part of the chest contributing to an aesthetical result that the patient can appreciate more.
Different authors have proposed some variation of the technique using, newly designed bar like Yüksel et al. (33), or the insertion of the bar through a breach in the thoracic cavity as Kálmán and Hock (34,35). Tarhan et al. in 2018 proposed a technique which combines intra and extrathoracic manoeuvres: he performs two bilateral incision to the thorax. Under endoscopic view, an introducer is insert into the thorax and then guided through an intercostal space out of the thorax again on the other side. Another presternal incision is made and nylon threads are attached to the introducer bilaterally. At this point a metal bar can be placed following the nylon threads and stabiliser are fixed without fasten it on the ribs (36).
Notwithstanding this surgery is proposed to young patient to treat a usually benign pathology, it is not immune to complication. These can include, depending on the chosen method: skin irritation, bleeding, displacement of the bar and infection of the scar and pneumothorax.
Discussion
Pectus carinatum is a chest wall deformity which usually do not cause physical effects, such as cardiac or lung compression. Often, the treatment regards the physical appearance and the psychological aspect. The severity of the malformation and the self-esteem can condition social and psychological life of the patient. Depending on this the treatment is tailored.
In our Centre, if the patient is under the age of ten, we only recommend observation. Even Fonkalsrud (37) in his last review concerning the correction of PC, affirm that he prefers to avoid surgical correction in children under the age of 11 because of major technical problem and higher risk to develop a recurrence if severe or symptomatic deformities are not present (7).
As the child grows, we propose brace for those patients with the chondrogladiolar form. In this case it is very important patient’s compliance considering the duration and the dedication required for the treatment. If the device is not bear but the patient does not accept the deformity, we offer the possibility to undergo surgery, using the modified Ravitch technique. For this type of surgery, we prefer that the patient has reached an adequate physical development. Therefore, due to the fact that in these cases the chest wall does not have any more a big compliance, we do not perform minimally invasive procedures. The description made by Fonkalsrud (37) of 260 cases of PC executed with open methods, shows that even these techniques cause nowadays less chest wall demolition.
Through the review of the literature, the correct patient selection is extremely important to obtain the best result. Nowadays, patients have many alternative treatments, invasive and not-invasive procedures, that’s why counseling is becoming more and more important. Patients who want to treat their condition, should turn to a dedicated Centre with good expertise in the management of this kind of chest wall malformations.
Acknowledgments
We would like to express our gratitude to Doctor Marco Scarci for his cooperation in providing the photographic material.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Paolo Scanagatta) for the series “Pediatric Thoracic Surgery” published in Pediatric Medicine. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/pm.2019.05.02). The series "Pediatric Thoracic Surgery" was commissioned by the editorial office without any funding or sponsorship. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Oncel M, Tezcan B, Akyol KG, et al. Clinical experience of repair of pectus excavatum and carinatum deformities. Cardiovasc J Afr 2013;24:318-21. [Crossref] [PubMed]
- Emil S, Laberge JM, Sigalet D, et al. Pectus carinatum treatment in Canada: current practices. J Pediatr Surg 2012;47:862-6. [Crossref] [PubMed]
- Willital GH, Lehmann RR. Surgery in Childhood, 33-67. In: Chirurgie im Kindesalter Gebundenes Buch – 1. Januar 2000. Balingen: Spitta Verlag, 2000.
- Willital GH, Saxena AK, Shütze U, et al. Chest-deformities: a proposal for a classification. World J Pediatr 2011;7:118-23. [Crossref] [PubMed]
- Chidambaram B, Mehta AV. Currarino-Silverman syndrome (pectus carinatum type 2 deformity) and mitral valve disease. Chest 1992;102:780-2. [Crossref] [PubMed]
- Haller JA Jr, Kramer SS, Lietman SA. Use of CT scans in selection of patients for pectus excavatum surgery: a preliminary report. J Pediatr Surg 1987;22:904-6. [Crossref] [PubMed]
- Fonkalsrud EW, Mendoza J. Open repair of pectus excavatum and carinatum deformities with minimal cartilage resection. Am J Surg 2006;191:779-84. [Crossref] [PubMed]
- Emil S. Current Options for the Treatment of Pectus Carinatum: When to Brace and When to Operate? Eur J Pediatr Surg 2018;28:347-54. [Crossref] [PubMed]
- Koumbourlis AC. Pectus deformities and their impact on pulmonary physiology. Paediatr Respir Rev 2015;16:18-24. [Crossref] [PubMed]
- Steinmann C, Krille S, Mueller A, et al. Pectus excavatum and pectus carinatum patients suffer from lower quality of life and impaired body image: a control group comparison of psychological characteristics prior to surgical correction. Eur J Cardiothorac Surg 2011;40:1138-45. [PubMed]
- Vidal J, Perdriolle R, Brahin B, et al. Conservative treatment of deformities of the anterior chest wall Rev Chir Orthop Reparatrice Appar Mot 1977;63:595-608. (in French). [PubMed]
- Haje SA, Bowen JR. Preliminary results of orthotic treatment of pectus deformities in children and adolescents. J Pediatr Orthop 1992;12:795-800. [Crossref] [PubMed]
- Martinez-Ferro M, Fraire C, Bernard S. Dynamic compression system for the correction of pectus carinatum. Semin Pediatr Surg 2008;17:194-200. [Crossref] [PubMed]
- Lopez M, Patoir A, Varlet F, et al. Preliminary study of efficacy of dynamic compression system in the correction of typical pectus carinatum. Eur J Cardiothorac Surg 2013;44:e316-9. [Crossref] [PubMed]
- Sesia SB, Holland-Cunz S, Häcker FM. Dynamic compression system: an effective nonoperative treatment for pectus carinatum: a single center experience in Basel, Switzerland. Eur J Pediatr Surg 2016;26:481-6. [Crossref] [PubMed]
- de Beer SA, Gritter M, de Jong JR, et al. The dynamic compression brace for pectus carinatum: intermediate results in 286 patients. Ann Thorac Surg 2017;103:1742-9. [Crossref] [PubMed]
- Cohee AS, Lin JR, Frantz FW, et al. Staged management of pectus carinatum. J Pediatr Surg 2013;48:315-20. [Crossref] [PubMed]
- Emil S, Sévigny M, Montpetit K, et al. Success and duration of dynamic bracing for pectus carinatum: a four-year prospective study. J Pediatr Surg 2017;52:124-9. [Crossref] [PubMed]
- Kravarusic D, Dicken BJ, Dewar R, et al. The Calgary protocol for bracing of pectus carinatum: a preliminary report. J Pediatr Surg 2006;41:923-6. [Crossref] [PubMed]
- Frey AS, Garcia VF, Brown RL, et al. Nonoperative management of pectus carinatum. J Pediatr Surg 2006;41:40-5. [Crossref] [PubMed]
- Lee SY, Lee SJ, Jeon CW, et al. Effect of the compressive brace in pectus carinatum. Eur J Cardiothorac Surg 2008;34:146-9. [Crossref] [PubMed]
- Pessanha I, Severo M, Correia-Pinto J, et al. Pectus Carinatum Evaluation Questionnaire (PCEQ): a novel tool to improve the follow-up in patients treated with brace compression. Eur J Cardiothorac Surg 2016;49:877-82. [Crossref] [PubMed]
- Kang DY, Jung J, Chung S, et al. Factors affecting patient compliance with compressive brace therapy for pectus carina- tum. Interact Cardiovasc Thorac Surg 2014;19:900-3. [Crossref] [PubMed]
- Desmarais TJ, Keller MS. Pectus carinatum. Curr Opin Pediatr 2013;25:375-81. [Crossref] [PubMed]
- Ravitch MM. Unusual sternal deformity with cardiac symptoms–operative correction. J Thorac Surg 1952;23:138-44. [PubMed]
- Ravitch MM. The operative correction of pectus carinatum (pigeon breast). Ann Surg 1960;151:705-14. [Crossref] [PubMed]
- Robicsek F, Sanger PW, Taylor FH, et al. The surgical treatment of chondrosternal prominence (pectus carinatum). J Thorac Cardiovasc Surg 1963;45:691-701. [PubMed]
- Scarci M, Bertolaccini L, Panagiotopoulos N, et al. Open repair of pectus carinatum. J Vis Surg 2016;2:50. [Crossref] [PubMed]
- Del Frari B, Sigl S, Schwabegger AH. Complications related to pectus carinatum correction: lessons learned from 15 years’ experience. Management and literature review. Plast Reconstr Surg 2016;138:317e-29e. [Crossref] [PubMed]
- Muntean A, Stoica I, Saxena AK. Pigeon chest: comparative analysis of surgical techniques in minimal access repair of pectus carinatum (MARPC). World J Pediatr 2018;14:18-25. [Crossref] [PubMed]
- Kobayashi S, Yoza S, Komuro Y, et al. Correction of pectus excavatum and pectus carinatum assisted by the endoscope. Plast Reconstr Surg 1997;99:1037-45. [Crossref] [PubMed]
- Abramson H. A minimally invasive technique to repair pectus carinatum. Preliminary report. Arch Bronconeumol 2005;41:349-51. [PubMed]
- Yüksel M, Bostanci K, Evman S. Minimally invasive repair of pectus carinatum using a newly designed bar and stabilizer: a single institution experience. Eur J Cardiothorac Surg 2011;40:339-42. [PubMed]
- Kálmán A. Initial results with minimally invasive repair of pectus carinatum. J Thorac Cardiovasc Surg 2009;138:434-8. [Crossref] [PubMed]
- Hock A. Minimal access treatment of pectus carinatum: a preliminary report. Pediatr Surg Int 2009;25:337-42. [Crossref] [PubMed]
- Tarhan T, Maurer A, Tarhan O. Combined extra-/intrathoracic correction of pectus carinatum and other symmetric chest wall deformities Oper Orthop Traumatol 2018;30:469-78. [Crossref] [PubMed]
- Fonkalsrud EW. Surgical correction of pectus carinatum: lessons learned from 260 patients. J Pediatr Surg 2008;43:1235-43. [Crossref] [PubMed]
Cite this article as: Rimessi A, Mazzucco A, Fieschi S, Torre M. Narrative review of therapeutical options in pectus carinatum in young patients. Pediatr Med 2019;2:17.