
Thinking uniportal in pediatric thoracic surgery
Introduction
The first experience in humans in minimal thoracic invasive surgery was reported in 1910 by Jacobaeus and consisted in placing an ureteroscope into the thoracic cavity to inspect the pleura and divide the adhesions in patients with tuberculosis (1,2). Later, Jacobeus reported the first significant experience with a series of 100 patients (3). In 1992 multiportal video-assisted thoracoscopic surgery (VATS) was developed in the field of thoracic surgery and during a 20-year time-span the multiportal approach has gradually expended (1). Conventional VATS was initially performed by 3–4 ports and it has become gold standard technique for most of thoracic surgical diseases. It started to evolve from three-ports to double-port and it was in the 2000s when the uniportal technique was defined. In 2004, uniportal VATS technique was described by Rocco et al. (4), limited to diagnostic procedures and pneumothorax treatment. Nowadays, the procedure widely extended in thoracic surgery in adults. Gonzalez et al. reported in 2011 the first mayor pulmonary resection by uniportal VATS applied to a lobectomy (5). In recent years, multiple publications have confirmed that this technique is achievable for a broad variety of complex thoracic procedures such as tracheal resection and reconstruction, bronchoplastic procedures, esophagectomies, and resection of advanced lung neoplasms with satisfactory outcomes (6-10), therefore, uniportal VATS is one of the greatest advances in the history of thoracic surgery in the last 10 years (1).
Single port technique has demonstrated clear advantages in adult population about mortality, morbidity and pain control compared to thoracotomy, with a better cosmetic result if compared to multiportal approach (11-14). However, the application of this technique in paediatric population is not widespread and reports in literature are limited.
Paediatric thoracic surgery includes a high variety of congenital, infectious and tumoral pathologies. Classic approach of these paediatric diseases was open thoracotomy. In the last decades, minimal invasive procedures have demonstrated being feasible and safe in multiple pathologies. In the 1970s and 1980s the first significant thoracoscopic experience in children was reported for biopsy procedures and empyema debridement (15). Since 1990s, due to technological revolution and expansion of laparoscopic surgery in adults, more advanced diagnostic and therapeutic procedures have been performed in children (16,17). Currently a large variety of indications are recognized for thoracoscopic operations in children (18). Thoracoscopic paediatric procedures varies from decortication for empyema and biopsy of intrathoracic lesions up to advanced procedures, such as repair of oesophageal atresia and resection of mediastinal masses (19).
However, uniportal approach is not extended in paediatric surgery and there are only a few cases reported in literature with satisfactory outcomes.
We present advantages and indications of uniportal VATS in children as well as a review of reported cases. We emphasize in the reproducibility and safety of single incision VATS in paediatric population in our clinical experience.
Technical considerations and limitations of uniportal VATS in paediatric population
A good understanding of anatomical characteristics in children are mandatory for a safe surgical procedure.
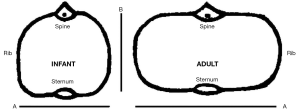
The morphology of the paediatric chest changes with age (Figure 1). In neonates, the thorax has a trapezoidal morphology and the ribs are horizontal with greater length in anteroposterior diameter. In the older children, the thorax is more rectangular and the vertical diameter is greater, resembling the adult’s chest (20). In addition, the child’s thorax is more flexible than in adults (21).
The diaphragm in children is positioned at a “higher level” than in adults. For this reason, diaphragm position should be considered when incisions are planned for thoracic surgery (22).
Working space is limited for VATS in children and the lung dimensions have to be taken into consideration as an issue when performing this technique. Lungs and airway in children are not fully developed at birth. The structural integrity of the airway improves after birth as the flexible cartilage of the infant’s larynx and trachea becomes more rigid (23). Single lung ventilation is more difficult in infant or small children if compared with adults. A double lumen-tube is too prominent for patients with less than 30 kg, however different options as bronchial blocker or selective intubation of the contralateral bronchus can be achieved (24). Ventilator-dependent patients and those with significant cardiac defects can tolerate a limited period of partial lung collapse necessary to perform most of thoracic procedures (25-27). Although it is mandatory to manage the retention of CO2 by modifying ventilatory parameters, a paediatric anaesthetist has to be able to perform this kind of surgeries.
Indications and limitations of uniportal VATS in paediatric surgery
Currently in thoracic surgery, thoracoscopy is the minimally invasive technique applied in most part of thoracic surgical interventions (26-28). The lack of evolution of uniportal VATS in pediatrics is explained by a low incidence of pathologies that require thoracic surgeries (29).
Several authors have reported their experience with uniportal VATS approach in different thoracic diseases in paediatric age with satisfactory outcomes (Table 1). In 2012, Aragón et al. reported the first surgical intervention by uniportal VATS in an 11-year-old paediatric patient (30). They performed a middle right lobectomy and lower right lobe resection without technical difficulties neither short-term complications.
Table 1
| Reference | Study type | Sex | Age | Comorbidities | Pathology | Incision | Procedure | Technical limitations | Complications |
|---|---|---|---|---|---|---|---|---|---|
| 2013, Aragón et al. (30) | Case report | Female | 11 years | Acute lymphoblastic leukemia | Pulmonary aspergilloma | 4 cm | Right middle lobectomy and wedge right lower lobe resection | No | No |
| 2016, Fernandez-Pineda et al. (31) | Case report | Male | 14 years | No | Bilateral lung nodules | 2.5–3 cm | Wedge resection (unspecified side) | No | No |
| Histoplasma capsulatum infection | |||||||||
| 2016, Gonzalez-Rivas et al. (29) | Case report | Female | 10 years | No | Endobronchial carcinoid tumor (blocking the entrance of the right upper bronchus) | 3 cm | Right upper sleeve lobectomy and tracheoplasty | No | No |
| Mediastinal lymphadenectomy | |||||||||
| 2016, Halezeroglu S et al. (32) | Case report | Male | 14 months | No | Extralobar pulmonary sequestration (over de left diaphragm) | 3 cm | Resection of sequestrated lung | Limited distance between the incision and the vascular bundle. The stapling device was not possible to work | No |
| 2018, Fortes et al. (33) | Case report | Male | 1 day | Premature (28 weeks, 1,040 g) | Type C esophageal atresia | 3 cm | Fistula ligation and end-to-end esophageal anastomosis | No | No |
| Female | 1 day | No | 3 cm | ||||||
| 2019, Fernandez-Pineda et al. (34) | Retrospective review | Male [n=6]; female [n=5] | Range: 7–21 years | Primary neoplasia | Lung nodule | 3 cm | Resection or biopsy | No | No |
VATS, video-assisted thoracoscopic surgery.
Most part of uniportal VATS procedures performed in paediatric surgery are minor procedures (26,27). Thoracic sympathectomy due to hyperhidrosis, pneumothorax, empyema decortication, biopsies and resection of lung nodes have been described in the literature.
Fernandez-Pineda et al. [2016] reported the first experience with this technique in a 14-year-old oncological patient with an infectious pulmonary nodule caused by Histoplasma capsulatum and resected by uniportal approach (31). Several years later they described their experience with a review of 11 patients with satisfactory outcomes (34).
A standardized use of uniportal VATS in paediatric patients for complex thoracic surgeries like mayor pulmonary resections or neonatal surgery is difficult to achieve. Nevertheless, uniportal VATS is safe and feasible if is performed by surgeons with experience in minimally invasive surgery (35,36). Gonzalez-Rivas et al. reported in 2016 a case of a 10-year-old patient with an endobronchial tumour. A right upper sleeve lobectomy and a tracheoplasty, and associated mediastinal lymphadenectomy was performed (29). According to our knowledge this is the most complex surgery performed by means of uniportal VATS in a paediatric population.
Another great challenge for the paediatric thoracic surgeon is neonatal pathology. As we discussed, the reduced space in these patients and anatomical characteristics in this age make more difficult the development of minimally invasive techniques.
Thoracoscopy has been limited in low weight patients due to both the reduced space in thorax and the absence of specific material for this age (18,22). Because of these difficulties, Rothenburg et al. reported 26 lobectomies for benign diseases where he determined the need of specific instruments adapted to paediatric patients (23). By the other hand, a few authors have reported their experiences with uniportal VATS in newborn patients. Our group previously reported [2018] the experience with a low weight premature who was treated with uniportal approach with satisfactory outcomes (33). A low birth weight neonate male of 1,040 grams born at 28 weeks with an esophageal atresia type C was presented. The patient underwent surgery by tracheo-esophagic fistula closure and esophagic anastomosis by uniportal VATS at 24 hours of life. Surgery developed without incidents and with excellent outcomes. Up to this point, four more cases with same pathology have been operated with the same technique by our group with better results than with conventional surgery.
Thoracic pathology in paediatric patient can be classified in three groups: infectious or acute pathology, congenital pathology and oncological pathology. Uniportal VATS seams a good alternative with multiples advantages to treat the most part of diseases of these three groups (Table 2). In adults, oncological indications are the most frequent for uniportal VATS surgery. By contrast, in paediatric patients oncological disease is less frequent because lung or pleural tumours are uncommon (29). Thoracic surgery is carried out in paediatric patients predominantly with benign indications. Infectious disease represents the most frequent cause of thoracic surgery in this age, followed by congenital pathology where neonatal pulmonary malformations are remarkable.
Table 2
| Indications | Uniportal VATS procedure |
|---|---|
| Congenital pathology | |
| Esophageal atresia | Anastomosis and fistula closure* |
| Esophageal duplication | Resection |
| Esophageal diverticula | Resection |
| Cystic adenomatoid malformation | Lobectomy or resection* |
| Pulmonary sequestration | Lobectomy or resection* |
| Bronchogenic cyst | Resection |
| Diaphragmatic hernia | Hernia closure |
| Diaphragmatic relaxation | Diaphragmatic plication |
| Pericardial cyst | Cyst resection |
| Acute pathology | |
| Diaphragmatic rupture | Diaphragmatic closure |
| Empyema | Decortication* |
| Pneumothorax | Pleurodesis* |
| Oncological pathology | |
| Solid neoplasm | Resection or biopsy or lobectomy* |
| Lung nodule | Resection or biopsy* |
| Others | |
| Palmar hydrosis | Sympathectomy* |
| Achalasia | Cardiomyotomy |
| Myasthenia gravis | Thymectomy |
| Chylothorax | Thoracic duct ligation |
*, intervened pathology by uniportal VATS. VATS, video-assisted thoracoscopic surgery.
In the last years, several variations to improve the original technique have been reported both for adults and children surgeries (34,37-42). Fernandez-Pineda et al. [2018] reported the approach by single port but with access through two intercostal spaces (camera trough upper intercostal space and instrumentation trough lower intercostal space) (34). With this approach, they conserved functional and aesthetic advantages of uniportal VATS, however camera mobility was not conditioned by instrumental mobility. Subxiphoid or infrasternal approach has also been reported by other authors as a new alternative to traditional uniportal VATS intercostal access (38,40-42). Through this incision thymectomies, lobectomies, even bipleural approaches have been reported. More and more paediatric patients can benefit from this advance.
Advantages of uniportal approach in pediatric thoracic surgery
Uniportal VATS offers advantages of a minimally invasive approach and it allows to treat most part of thoracic pathologies that require surgical management with an optimal result (43-46).
Although there are few reports in literature about uniportal VATS in paediatric age, several studies have already demonstrated unquestionable improvements that uniportal surgery offers in adult population (44).
The single incision approach generates less pain postoperative than conventional thoracotomy or multiport access (47). This improve early mobilization and early respiratory rehabilitation. Chest tube can be removed earlier after surgery. In addition, the decrease of postoperative pain accelerates extubation in the paediatric patients allowing to introduce fast track protocols in thoracic paediatric surgery with reduced hospitalization time (48,49).
The main disadvantage of open thoracic surgery in the paediatric patient is morbidity associated with thoracotomy. The risk of developing deformities like scoliosis, scapular winging and muscle weakness after thoracic surgery is high, because of the development of musculoskeletal and nervous structures, that is achieved during childhood, especially during the first two years of life (50-53). However, no thoracic deformities after uniportal VATS have been reported. Any damage to the innervation of serratus anterior muscle and no need costal resection have been described (51). In addition, aesthetic advantages of a single 2.5–5 cm incision are obvious compared to open thoracotomy or multiportal approach.
One of the main disadvantages or thoracoscopy in paediatric surgery is the lack of space in thoracic cavity. This, together with the low volume of thoracic pathology at this age, generates a longer learning curve and reduces the application of this technique to highly complex surgical teams.
However, more and more authors defend that uniportal VATS as an effective and reproducible method in most of thoracic surgeries. This technique offers a similar vision to open surgery because of direct thoracic access unlike thoracoscopy that offers an angular vision (42,54). In addition, in uniportal VATS, all surgeons are looking at the same screen in front of them (Figure 2). This position improves the surgical posture and facilitates manual movements because hand-eye coordination improves (44,55,56). The direct vision makes manual movements similar to open surgery and learning curve is shorter that in multiportal approach (43,44,46,57).

Conclusions
The multiple advantages described for uniportal VATS have determined an increase of use in paediatric surgery in the last years. This approach allows a direct access to thoracic cavity with less morbidity than open surgery. In addition, its direct vision offers less technical difficulty than multiportal thoracoscopic surgery. Despite of this, the learning curve for the application of this technique in children is higher than in adults due to the lower incidence of thoracic pathology and the size of the thoracic cavity of the children. Consequently, only in high complex services of paediatric surgery this technique should be used.
One of the greatest challenges for paediatric surgeons has always been to adapt adult surgical techniques to paediatric and neonatal surgery. Due to the current advances in uniportal VATS, more and more paediatric pathologies are approached by this technique and more paediatric patients can benefit from its advantages.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Paolo Scanagatta) for the series “Pediatric Thoracic Surgery” published in Pediatric Medicine. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/pm.2019.04.03). The series “Pediatric Thoracic Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mineo TC, Ambrogi V. A glance at the history of uniportal video-assisted thoracic surgery. J Vis Surg 2017;3:157. [Crossref] [PubMed]
- Moisiuc FV, Colt HG. Thoracoscopy: origins revisited. Respiration 2007;74:344-55. [Crossref] [PubMed]
- Jacobeus HC. The practical importance of thoracoscopy in surgery of the chest. Surg Gynecol Obstet 1922;34:289-96.
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Guido-Guerrero W, Bolaños-Cubillo A, González-Rivas D. Single-port video-assisted thoracic surgery (VATS) - advanced procedures & update. J Thorac Dis 2018;10:S1652-61. [Crossref] [PubMed]
- Liu Z, Yang R, Shao F. Uniportal Video-Assisted Thoracoscopic Tracheal Resection. Ann Thorac Oncol Res 2017;1:1004.
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Dmitrii S, Pavel K. Uniportal Video-Assisted Thoracic Surgery Esophagectomy. Thorac Surg Clin 2017;27:407-15. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Single incision thoracoscopic right upper lobectomy with chest wall resection by posterior approach. Innovations 2013;8:70-2. [PubMed]
- Desai H, Natt B, Kim S, et al. Decreased In-Hospital Mortality after Lobectomy Using Video-assisted Thoracoscopic Surgery Compared with Open Thoracotomy. Ann Am Thorac Soc 2017;14:262-6. [PubMed]
- Bendixen M, Jørgensen OD, Kronborg C, et al. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol 2016;17:836-44. [Crossref] [PubMed]
- Jawitz OK, Wang Z, Boffa DJ, et al. The differential impact of preoperative comorbidity on perioperative outcomes following thoracoscopic and open lobectomies. Eur J Cardiothorac Surg 2017;51:169-74. [Crossref] [PubMed]
- Reinersman JM, Passera E, Gaetano Rocco G. Overview of uniportal video-assisted thoracic surgery (VATS): past and present. Ann Cardiothorac Surg 2016;5:112-7. [Crossref] [PubMed]
- Rodgers BM, Moazam F, Talbert JL. Thoracoscopy in children. Ann Surg 1979;189:176-80. [Crossref] [PubMed]
- Rodgers BM. Pediatric thoracoscopy: where have we come and what have we learned? Ann Thorac Surg 1993;56:704-7. [Crossref] [PubMed]
- Rothenberg SS, Wagner JS, Chang JH, et al. The safety and efficacy of thoracoscopic lung biopsy for diagnosis and treatment in infants and children. J Pediatr Surg 1996;31:100-3. [Crossref] [PubMed]
- Engum SA. Minimal access thoracic surgery in the pediatric population. Semin Pediatr Surg 2007;16:14-26. [Crossref] [PubMed]
- Rothenberg SS. Thoracoscopy in infants and children. In: Holcomb GW III, Murphy JP, Ostlie DJ. editors. Ashcraft’s pediatric surgery. 5th edition. Philadelphia: Saunders 2010:362-75.
- García Asensio D, Fernández Martín M. Pitfalls and variants in pediatric chest imaging. Radiologia 2016;58:58-69. [PubMed]
- Rokitansky A. Thorax. In: Zachariou Z. editor. Pediatric Surgery Digest. 1st edition. Berne, Switzerland: Springer-Verlag Berlin Heidelberg, 2009:227.
- Fischer NJ, Morreau J, Sugunesegran R, et al. A Reappraisal of Pediatric Thoracic Surface Anatomy. Clin Anat 2017;30:788-94. [Crossref] [PubMed]
- Rothenburg S. Thoracoscopic lobectomy in infants and children utilizing a 5 mm stapling devide. J Laparoendosc Adv Surg Tech 2016;26:1036-8. [Crossref]
- Bax K. editor. Thoracoscopy. In: Pediatric Surgery: Diagnosis and Management. Puri P, Höllwarth ME. editors. 1st edition. Dublin, Ireland: Springer-Verlag Berlin Heidelberg, 2006.
- Rothenberg S. Thoracoscopy-basic techniques. In: Najmaldin A, Rothenberg S, Crabe D, et al. editors. Operative endoscopy and endoscopic surgery in infants and children. 1st edition. London: CRC Press, 2005.
- Oak SN, Parelkar SV, Satishkumar KV, et al. Review of video-assisted thoracoscopy in children. J Minim Access Surg 2009;5:57-62. [Crossref] [PubMed]
- Martínez-Ferro M, Duarte S, Laje P. Single Port Thoracoscopy for the Treatment of Pleural Empyema in Children. J Pediatr Surg 2004;39:1194-6. [Crossref] [PubMed]
- Zoeller C, Ure BM, Dingemann J. Perioperative Complications of Video-Assisted Thoracoscopic Pulmonary Procedures in Neonates and Infants. Eur J Pediatr Surg 2018;28:163-70. [Crossref] [PubMed]
- Gonzalez-Rivas D, Marin JC, Granados JP, et al. Uniportal video-assisted thoracoscopic right upper sleeve lobectomy and tracheoplasty in a 10-year-old patient. J Thorac Dis 2016;8:E966-9. [Crossref] [PubMed]
- Aragón J, Pérez I. First Case Report of Single Port Video-Assisted Thoracoscopic Middle Lobectomy for the Treatment of Pulmonary Aspergilloma in a Pediatric Patient. European J Pediatr Surg Rep 2013;1:12-4. [Crossref] [PubMed]
- Fernandez-Pineda I, Seims AD. Modified uniportal video-assisted thoracic surgery in children. J Minim Access Surg 2016;12:373-4. [Crossref] [PubMed]
- Halezeroğlu S, Okur E, Ergene G. Single-Incision Video-Assisted Thoracic Surgery for an Extralobar Sequestration in a Child. Innovations (Phila) 2016;11:64-6. [PubMed]
- Míguez L, García M, Curros N, et al. A new uniportal approach on treatment of esophageal atresia: uniportal vats for surgical repair-a report of two cases. Ann Pediatr Surg 2018;14:95-7. [Crossref]
- Fernandez-Pineda I, Seims AD, VanHouwelingen L, et al. Modified Uniportal Video-Assisted Thoracic Surgery Versus Three-Port Approach for Lung Nodule Biopsy in Pediatric Cancer Patients. J Laparoendosc Adv Surg Tech A 2019;29:409-14. [Crossref] [PubMed]
- Guido W, González-Rivas D, Duang L, et al. Uniportal video-assisted thoracoscopic right upper sleeve lobectomy. J Vis Surg 2015;1:10. [PubMed]
- Reinersman JM, Pasera E, Rocco G. Overview of uniportal video-assisted thoracic surgery (VATS): past and present. Ann Cardiothorac Surg 2016;5:112-7. [Crossref] [PubMed]
- Gigirey Castro O, Berlanga G, Sánchez E. Single Port Thorascopic Surgery Using the SILS® Tool as a Novel Method in the Surgical Treatment of Pneumothorax. Arch Bronconeumol 2010;46:439-41. [Crossref] [PubMed]
- Carvalheiro C, Gallego J, González-Rivas D, et al. Uniportal VATS lobectomy: subxiphoid approach. Rev Port Cir Cardiotorac Vasc 2017;24:141. [PubMed]
- Shibuya S, Nakamura T, Miyazaki E. Anatomical Segmentectomy with a Hybrid VATS Approach in a Patient with Intralobar Pulmonary Sequestration after Severe Pneumonia: A Case Report. European J Pediatr Surg Rep 2017;5:e21-5. [Crossref] [PubMed]
- Suda T, Sugimura H, Tochii D. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. [Crossref] [PubMed]
- Suda T, Ashikari S, Thochii D. Single-incision subxiphoid approach for bilateral metastasectomy. Ann Thorac Surg 2014;97:718-9. [Crossref] [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxyphoid single-incision thoracoscopic pulmonary metastasectomy. Thorac Cancer 2015;6:230-2. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Nachira D, Meacci E, Ismail M, et al. Why to change from multiportal to uniportal VATS? Video-assist Thorac Surg 2018;3:14. [Crossref]
- Wang L, Liu D, Lu J, et al. The feasibility and advantage of uniportal video-assisted thoracoscopic surgery (VATS) in pulmonary lobectomy. BMC Cancer 2017;17:75. [Crossref] [PubMed]
- Drevet G, Ugalde P. Uniportal video-assisted thoracoscopic surgery: safety, efficacy and learning curve during the first 250 cases in Quebec, Canada. Ann Cardiothorac Surg 2016;5:100-6. [Crossref] [PubMed]
- Karnik PP, Dave NM, Garasia M. Comparison of analgesic efficacy and safety of continuous epidural infusion versus local infiltration and systemic opioids in video-assisted thoracoscopic surgery decortication in pediatric empyema patients. Saudi J Anaesth 2018;12:240-4. [Crossref] [PubMed]
- Kugler C. Minimal-invasive thoracic surgery in pediatric patients. J Vis Surg 2018;4:10. [Crossref] [PubMed]
- Clermidi P, Bellon M, Skhiri A, et al. Fast track pediatric thoracic surgery: Toward day-case surgery? J Pediatr Surg 2017;52:1800-5. [Crossref] [PubMed]
- Panda SS, Agarwala S, Bhatnagar V, et al. A survey of musculoskeletal and aesthetic abnormalities after thoracotomy in pediatric patients. J Indian Assoc Pediatr Surg 2013;18:136-42. [Crossref] [PubMed]
- Bleiziffer S, Schreiber C, Burgkart R, et al. The influence of right antero-lateral thoracotomy in prepubescent female patients on late breast development and on the incidence of scoliosis. J Thorac Cardiovasc Surg 2004;127:1474-80. [Crossref] [PubMed]
- Akçali Y, Demir H, Tezcan B. The effect of standard posterolateral versus muscle-sparing thoracotomy on multiple parameters. Ann Thorac Surg 2003;76:1050-4. [Crossref] [PubMed]
- Rothenberg SS, Pokorny WJ. Experience with a total muscle-sparing approach for thoracotomies in neonates, infants and children. J Pediatr Surg 1992;27:1157-9. [Crossref] [PubMed]
- Ismail M, Swierzy M, Nachira D, et al. Uniportal video-assisted thoracic surgery for major lung resections: pitfalls, tips and tricks. J Thorac Dis 2017;9:885-97. [Crossref] [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5:S214-6. [PubMed]
- Bertolaccini L, Viti A, Terzi A, et al. Geometric and ergonomic characteristics of the uniportal video-assisted thoracoscopic surgery (VATS) approach. Ann Cardiothorac Surg 2016;5:118-22. [Crossref] [PubMed]
- Bedetti B, Bertolaccini L, Solli P, et al. Learning curve and established phase for uniportal VATS lobectomies: the Papworth experience. J Thorac Dis 2017;9:138-42. [Crossref] [PubMed]
Cite this article as: Casal-Beloy I, Míguez Fortes L, Gómez Tellado MA, González-Rivas D. Thinking uniportal in pediatric thoracic surgery. Pediatr Med 2019;2:13.

