
Robotic thoracic surgery in children and adolescents—technology and adaptability
Robotic surgery for pediatric patients has been described since at least 2001 (1), and the robotic platform has been increasingly used in pediatric gastrointestinal, genitourinary, and solid tumor resections (2,3). However, the number of pediatric minimally-invasive thoracic procedures utilizing the robotic platform remains smaller versus other surgical subspecialty procedures (4). The robot is not suitable for most children that are 2 years of age or younger due to their diminutive size and smaller rib interspaces. Other factors influencing the utilization of the robotic platform in pediatric thoracic surgery include: (I) smaller chest walls in children limiting port placement and access, (II) hesitancy to adapt new technology to a delicate patient cohort, and (III) the overall cost of the robotic system (5). Perhaps the most significant reason is the training of the typical pediatric surgeon, which has in the past been commonly devoid of robust robotic training in general surgical residency. This is also coupled with the fact that in most academic institutions, pediatric thoracic operations are performed by pediatric surgeons and not thoracic surgeons, who may be more familiar with the robotic platform. More commonly the expertise of the two subspecialties are combined.
With careful patient selection, a supportive robotic and pediatric surgical team, and a detailed understanding of thoracic anatomy and physiology, the da Vinci® robotic platform (Intuitive Surgical Inc., Sunnyvale, CA, USA) can be easily adapted to fit selected pediatric patients.
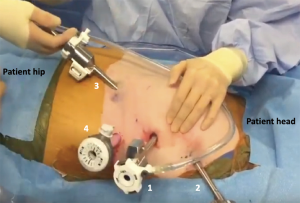
The pediatric thoracic procedures we have found to be most ideal for adaptation to the robotic platform include thymectomy (6), pulmonary sequestration resection and pulmonary metastasectomy. We have now performed 293 pediatric thoracic operations of which approximately 115 are robotic. Figure 1 illustrates the da Vinci® Xi port placement for a robotic thymectomy in a 10-year-old adolescent with myasthenia gravis. In general, we prefer to use the da Vinci® Si robot that it has 5-mm ports (an advantage in smaller pediatric patients) whereas the newer Xi robot has only 8 mm and larger ports.
We believe that a pediatric patient’s height is a surrogate for chest wall circumference and therefore the robotic platform should be appropriate even for children under three feet (91 cm) tall. We do not have a strict exclusionary height criteria for our pediatric patients. There are case reports describing smaller patients—even infants and neonates (7) however this may be more appropriate for abdominal operations such as genitourinary and general surgical procedures where abdominal insufflation creates more space for port clearance. In these smaller patients or newborns, we have used, similar to others (4), a video-assisted platform or (if required) thoracotomy and a cervical incision for procedures such as sliding tracheoplasty.
We have performed the vast majority of our elective pediatric operations during the summer months in order to mitigate or eliminate time out of school. The optimal operative timing needs to be carefully considered in the pediatric patient cohort. Robotic pulmonary resections usually only require two weeks or less for full recovery unlike more complex procedures such as congenital heart operations. In general, children recover quicker than most adults and are able to resume full physical activity in 2–3 weeks after robotic thoracic surgery.
We have performed many robotic operations in children. The most common operations we have performed are: lobectomy for sequestration, segmentectomy and/or wedge resection for metastatic disease (more commonly though we use a video-assisted platform for wedge resection), lobectomy for larger tumors, thymectomy (most commonly for myasthenia gravis), resection of esophageal duplication cysts, removal of neurilemoma/schwannoma, and others. These operations are exceedingly safe and effective. We have experienced no conversions, no blood transfusions, a median hospital length of stay of 1 day (range, 0–5 days), avoidance of the pediatric intensive care unit, and most importantly, no 30- or 90-day mortalities (8).
In conclusion, we believe that the robotic platform provides a safe and effective minimally-invasive platform for selected pediatric patients and surgical teams. The earlier outcomes have been spectacular in our experience. A video of the proper and thoughtful port placement as well as the conduct of a pediatric robotic left-sided thymectomy can be found here: https://www.youtube.com/watch?v=smfsWMBxf6M&t=2s.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Paolo Scanagatta) for the Series “Pediatric Thoracic Surgery” published in Pediatric Medicine. The article has undergone external peer review.
Conflicts of Interest: The Series “Pediatric Thoracic Surgery” was commissioned by the editorial office without any funding or sponsorship. Dr. Cerfolio discloses relationships with Bovie, Community Health Services, Covidien/Medtronic, C-SATS, Davol/Bard, Ethicon, Google/Verb, Intuitive Surgical, KCI/Acelity Company, Myriad Genetics, Pinnacle, ROLO-7 Consulting Firm and TEGO Corporation. Dr. Ferrari-Light has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Meininger DD, Byhahn C, Heller K, et al. Totally endoscopic Nissen fundoplication with a robotic system in a child. Surg Endosc 2001;15:1360. [Crossref] [PubMed]
- Cundy TP, Shetty K, Clark J, et al. The first decade of robotic surgery in children. J Pediatr Surg 2013;48:858-65. [Crossref] [PubMed]
- Cundy TP, Marcus HJ, Clark J, et al. Robot-assisted minimally invasive surgery for pediatric solid tumors: a systematic review of feasibility and current status. Eur J Pediatr Surg 2014;24:127-35. [PubMed]
- Ballouhey Q, Villemagne T, Cros J, et al. Assessment of paediatric thoracic robotic surgery. Interact Cardiovasc Thorac Surg 2015;20:300-3. [Crossref] [PubMed]
- de Lambert G, Fourcade L, Centi J, et al. How to successfully implement a robotic pediatric surgery program: lessons learned after 96 procedures. Surg Endosc 2013;27:2137-44. [Crossref] [PubMed]
- Hartwich J, Tyagi S, Margaron F, et al. Robot-assisted thoracoscopic thymectomy for treating myasthenia gravis in children. J Laparoendosc Adv Surg Tech A 2012;22:925-9. [Crossref] [PubMed]
- Kim SJ, Barlog JS, Akhavan A. Robotic-Assisted Urologic Surgery in Infants: Positioning, Trocar Placement, and Physiological Considerations. Front Pediatr 2019;6:411. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Minnich DJ. Starting a robotic program in general thoracic surgery: why, how, and lessons learned. Ann Thorac Surg 2011;91:1729-36; discussion 1736-7.
Cite this article as: Ferrari-Light D, Cerfolio RJ. Robotic thoracic surgery in children and adolescents—technology and adaptability. Pediatr Med 2019;2:11.

