Sustainable implementation of early intervention for autism spectrum disorder through caregiver coaching: South African perspectives on barriers and facilitators
Introduction
The estimated global prevalence of autism spectrum disorder (ASD) is 1 in 160 people (1). However, there is limited data on ASD in many parts of the world (2). In sub-Saharan Africa (SSA), where over 1 billion people live, no population-based prevalence studies have been conducted, and there is minimal empirical data on ASD phenotype, etiology, and intervention (2,3). Yet most at-risk children live in this part of the world (4,5).
In a 2017 scoping review, Franz and colleagues identified eleven ASD intervention studies in SSA (2). None of these publications explored the development or implementation of early ASD interventions on the continent (2). Studies conducted in high-income countries, where the preponderance of early ASD interventions have been developed, suggest that early intensive behavioral intervention can reduce core ASD symptom severity and costs associated with education and related social supports (6-11). There is agreement that caregiver education and skills training should occur following an ASD diagnosis (12).
Specialist providers typically implement early ASD intervention, which is problematic in most low and middle-income countries (LMICs), given that access to specialist care is so limited (13,14). In countries such as South Africa, there is growing recognition that specialist providers cannot address population needs for early ASD intervention (15). For this reason, involving caregivers of young children with ASD in treatment delivery is likely to be an important potential early intervention implementation strategy.
In a meta-analysis, Reichow and colleagues examined psychosocial interventions by ‘non-specialist providers’ for children who had intellectual disability or ‘lower-functioning’ ASD (16). Only two of the studies with young child with ASD included in this meta-analysis were conducted in a LMIC. In these two studies from China, ‘non-specialists’ were qualified teachers and community therapists who provided intervention directly to the child, without caregiver involvement (17,18). To our knowledge, to date, three published studies have examined Naturalistic Developmental Behavioral Intervention (NDBI)-informed caregiver coaching approaches in LMICs (19-21). NDBIs comprise a class of proven ASD early intervention approaches that aim is to enhance communication and social interaction by capitalizing on a child's motivations and interests (22). These intervention approaches can be taught to caregivers (22). While two of these studies, conducted in India, Pakistan and China (19,20) reported improvements in child and caregiver outcomes, caregiver coaches had at least a university-level Bachelor’s degree. This workforce is unlikely to be scalable in low-resource environments. In the third study, conducted in India lay health workers under the supervision of specialists, delivered a 12-session caregiver coaching intervention (21). While this study provides preliminary evidence of the feasibility and effectiveness of a non-specialist delivered early ASD intervention in India, contextual implementation challenges are likely to be different in other LMICs (23).
Despite South Africa being an upper middle income country (24), it has the highest GINI coefficient making it the world’s most unequal country (25). The needs of the vast majority of the population requiring early ASD intervention go unmet (23,26). This is true across the country, including in the Western Cape Province which is thought of as one of the better-resourced in terms of healthcare and education (26,27). This is due to a combination of factors, including: (I) limited ASD government services, for example, there are nine government funded ASD schools in South Africa for a population of over 52 million people; (II) most people live in poverty. More than half of South Africans live on less than 992 South African Rand (approximately USD$78) per person per month (27). This significantly impacts South Africans ability to pay out of pocket for private services; and (III) while private services may be available in some urban centers, they are expensive, vary in quality, and likely not evidence-based (28). Having a disability, living in poverty, and the legacy of apartheid on people of color therefore act as barriers to accessing existing education and health services (29-31). Springer and colleagues documented racial variations in expressive language abilities at diagnosis in one of the few studies of ASD phenotype in South Africa (29). In their study, a significantly greater number of black African children (94%) were non-verbal at diagnosis, as compared to Caucasian children (42%) (29). Importantly, the unmet need for early ASD intervention is increasing. There has been a 276% rise in the number of children with ASD on the waiting list for special education services in the Western Cape Province, 70% of whom are under 7 years of age (32).
Early ASD intervention research is beginning in South Africa at the University of Cape Town (33). In one of these studies, pilot work is underway on the Early Start Denver Model (ESDM), which is an NDBI (34). This study aims to adapt and implement a non-specialist delivered caregiver coaching version of ESDM, sensitized to the South African context, and integrated into existing systems of care (23,26,35). ESDM-informed coaching was chosen because there was already interest and activity related to the model in South Africa. Therapists had received some training in ESDM, and the US-based investigator was at an academic medical center where ESDM training occurred.
The Consolidated Framework for Implementation Research (CFIR) is the implementation science framework that informed intervention tailoring for the South African context (36). CFIR defines the outer setting, inner setting, and delineates the individuals involved in intervention implementation. Information on the outer setting (economic, policy environment, and cultural/social context), inner setting (structural and cultural context), and individuals involved (organization leaders, local supervisors, non-specialist workers, caregivers who receive the intervention, and caregiver-child dyads) was gained through qualitative interviews with multi-level stakeholders (23,26,35). Through developing an understanding of these three environmental layers, the intervention approach was tailored to enhance contextual ‘fit’ and identify implementation partners.
In South Africa, Early Childhood Development (ECD) is an emerging priority area supported by national policy (37). The National Integrated Early Childhood Development Policy recognizes the South African governments “responsibility to ensure a sufficient number of appropriately qualified human resources, including ECD practitioners and their supervisors, to facilitate center- and non-center-based ECD programmes, including parent support programs (37).” ECD practitioners are therefore a non-specialist workforce that can be targeted for intervention implementation.
Formative work with senior management level stakeholders, in Health, Education, and Social Development, and the non-profit sector in the Western Cape Province identified that early ASD intervention was more closely aligned with Education Department goals than with Health or Social Development goals (26). Therefore, the Western Cape Education Department was identified as an implementation partner. Some Education Department ASD schools employ ECD practitioners, the non-specialist workforce supported by national policy. These practitioners typically provide services in a group setting with very limited reach (1 ECD practitioner for a class of 4 students). With only nine government funded ASD schools in South Africa (population 52 million), and long wait lists for ASD school enrollment (32), intervention services provided in this limited group setting has minimal impact. Implementation partner schools in the Western Cape were therefore open to exploring caregiver coaching, as a means to extend early intervention services to the vast majority of children not enrolled in school, but waiting for school placement and receiving no services.
As efforts to implement early ASD intervention increase in SSA, understanding implementation barriers and facilitators is essential for successful integration of these intervention approaches into routine care (38). Implementation of an early ASD intervention in a novel environment should be based on current knowledge about potentially effective treatment, combined with a systematic assessment of potential barriers and facilitators (39,40). This approach is critical because identification of context-specific barriers and facilitators may lead to certain implementation strategies (41). A qualitative process evaluation was therefore conducted to draw on the experiences of various stakeholders who participated in the initial implementation of the non-specialist-delivered, ESDM-informed caregiver coaching intervention in South (38). In this manuscript, we therefore examine barriers and facilitators to implement and sustain the intervention, with the goal of identifying implementation challenges and program and system strengths.
Methods
Participants
In-depth individual interviews were conducted with nine participants, recruited through purposive sampling. Participants included three South African certified ESDM therapists who functioned as ECD supervisors, two ECD practitioners and their direct school supervisors, and two caregivers and their young children with ASD who participated in the pre-pilot phase of the study (see Table 1). Both ECD supervisors were Head of Departments in their respective schools, had specific training in ASD, and many years of experience working with young children with ASD. While one of the ECD practitioners had many years of experience working with young children with ASD, the other ECD practitioners was in her first year post-ECD qualification and had just started to work with children with ASD. Study inclusion criteria for ESDM therapists: (I) certification as an ESDM therapist; and (II) participation in training and supervision of ECD practitioners. Study inclusion criteria for ECD practitioners and school supervisors: (I) employed by the Department of Education in a school that provides ECD services to children with ASD; (II) attendance of a four-day training; and (III) implementation of 12 sessions of caregiver coaching. Inclusion criteria for caregivers: (I) primary caregiver of a child with a confirmed diagnosis of ASD between the ages of 18 and 72 months; (II) speaks isiXhosa, Afrikaans or English; (III) lives within an area served by the Red Cross Neurodevelopmental clinic; and (IV) participates in 12 caregiver-coaching sessions.
Table 1
| Participant role | Gender | Race | Education level | Languages spoken |
|---|---|---|---|---|
| ESDM1 therapists | Female [3] | Black African [1]; Caucasian [2] | Tertiary | English & Afrikaans (all); Xhosa, Zulu, Sotho [1] |
| ECD2 school supervisors | Female [2] | Caucasian [2] | Tertiary | English & Afrikaans |
| ECD practitioners | Female [2] | Black African [1]; Colored3 [1] | ECD Certificate | English & Afrikaans (all); Xhosa [1] |
| Caregiver A | Male [1] | Colored [1] | Tertiary | English |
| Child A | Male [1], 5 yrs | Colored [1] | – | |
| Caregiver B | Female [1] | Colored [1] | Grade 12 | English |
| Child B | Male [1], 5 yrs | Indian [1] | – |
1ESDM, Early Start Denver Model; 2ECD, Early Childhood Development; 3Colored—A South African term used to describe people of mixed race.
Procedures
Ethical clearance was obtained from the University of Cape Town (HREC 039/2015), Duke University (IRB Pro00064533), and the Western Cape Education Department. Caregiver-coaching sessions occurred at two Western Cape Education Department schools, which employ non-specialist ECD practitioners and provide ASD-specific educational services for young children. Two ECD practitioners and their direct school supervisor attended a 4-day in-person training, led by a certified ESDM trainer and 3 South African ESDM therapists, where participants were introduced to concepts of caregiver coaching and ESDM strategies through “Help is in your hands” Community ESDM materials (Rogers SJ, Vismara L, Dawson G, et al. Help Is in Your Hands: A Web-Based Tool to Help Parents Build Their Toddlers’ Social and Communication Development 2017.). During the 4-day training ECD practitioners worked with a caregiver-child dyad to practice strategies they were being taught.
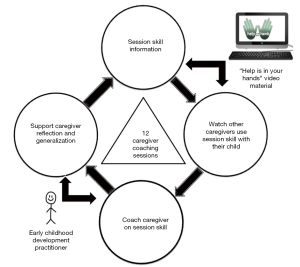
All data included in this manuscript is from the pre-pilot phase of a larger study. The purpose of the pre-pilot was to assess the feasibility of the intervention training and supervision approach and understand whether measures used to assess child clinical outcomes were sensitive to change. Two caregiver-child dyads, recruited to participate in the pre-pilot, received comprehensive baseline assessments. An ECD practitioner conducted twelve one-hour sessions of individual caregiver coaching. All coaching sessions occurred in a private space in the school, identified by our implementation partners. Figure 1 shows the structure of 12 sessions of caregiver coaching, where the session skill is introduced by “Help is in your hands” Community ESDM videos (Rogers SJ, Vismara L, Dawson G, et al. Help Is in Your Hands: A Web-Based Tool to Help Parents Build Their Toddlers’ Social and Communication Development 2017.). Session skills included specific strategies caregivers can use to increase their child’s attention to people and their child’s communication; strategies to identify, create and use joint activity routines to engage with and teach their child; in addition to ways to use the ABCs of learning to teach their child new behaviors. “Help is in your hands” Community ESDM materials also provide video examples of other caregivers using the session skill with their child. The ECD practitioner then coached the caregiver in the session skill, in at least two activities. The goal of coaching was to provide enough support for the caregiver to experience success in implementing the new skill with their child. Coaching was followed by caregiver reflection and a discussion of generalization of the new skill across various daily activities, using a daily activities visual aid. Given that this was the first time the ECD practitioner was coaching a caregiver-child dyad they were supported in-session by a certified ESDM therapist. The ESDM therapist’s role was primarily to ensure the ECD practitioner closely followed the session outline. Comprehensive follow up assessments were completed after the 12 coaching sessions.
Study methodology and individual interview questions were adapted from Curran and colleagues’ multi-stakeholder qualitative evaluation (38). See Table S1 for full interview guides. Interviews occurred after at least eight caregiver-coaching sessions in order to allow for participant familiarity with the coaching approach and session content. The interview guide varied slightly based on the participant group (see supplementary material for full interview guides). All interviews were in English, audio recorded and transcribed verbatim.
Data analysis
Qualitative data analysis followed the Braun and Clarke six-step process (42). Step one included reading/re-reading transcribed interviews. Step two consisted of hand-coding transcripts, line-by-line and assigning a code to a sentence/paragraph. Step three involved identifying patterns in the data, dividing the data up into categories, and labelling data according to themes. In step four, themes were reviewed under broad categories of barriers or facilitators of implementation and sustainability. Step five included naming, defining, and reorganizing themes and sub-themes under each category. In step six final analysis of the data was informed by the study aims and is represented in the results below. Study rigour was ensured through reflective journaling, peer debriefs and checking of the transcriptions by other team members for accuracy. The first author conducted steps one through three independently. Steps four through six were conducted by both the first author and the senior author, who reached consensus through regular sessions in which they reviewed themes, sub-themes and associated quotes.
Results
Table 2 summarizes themes and subthemes as they relate to barriers and facilitators to sustainable implementation of caregiver coaching.
Table 2
| Theme | Subtheme |
|---|---|
| Implementation facilitators | |
| ECD1 practitioner ASD2 knowledge and ongoing supervision | Baseline ASD knowledge |
| Ongoing supervision | |
| Positive coaching experience | Caregiver coaching structure |
| Strong team relationships | |
| Clear illustration of intervention concepts from the session videos | Illustration of intervention skills |
| Implementation barriers | |
| Intervention and coaching concepts | Complexity of concepts |
| Misalignment of ECD practitioner training with a caregiver coaching approach | |
| Logistical challenges | Time constraints |
| Access to physical resources | |
| Video content misaligned with South African context | Mismatch of material with the South African context |
| Facilitators to sustain the intervention | |
| Child and caregiver outcomes | Child outcomes |
| Caregiver ‘buy-in’ | |
| Caregiver competence | |
| Structural factors promoting intervention sustainability | Ongoing supervision |
| Feasibility within the school system | |
| Barriers to sustain the intervention | |
| Structural issues | Poverty, transportation, unemployment |
1ECD, Early Childhood Development; 2ASD, autism spectrum disorder.
Implementation facilitators
Implementation of caregiver coaching was facilitated by (I) ECD practitioner baseline knowledge and ongoing supervision; (II) a positive coaching experience; and (III) clear illustration of intervention concepts from the session videos.
ECD practitioner ASD knowledge and ongoing supervision
While some participants thought it was necessary to include ECD practitioners with prior ASD experience, with supervision ECD practitioners were able to learn intervention and coaching skills.
Baseline ASD knowledge
One of the ECD school supervisor commented:
“If our ECD practitioner had more experience with autism learners, I think she would be more comfortable if she knew more about autism.”
However, two certified ESDM therapists thought that a ‘novice’ ECD practitioner was more amenable to learning new skills:
“Because she is newer to it. I don’t think she’s had any formal training in autism. She is more receptive to information from us. You didn’t have to declutter, to get rid of stuff that she already knew, or ideas that she had about what she’d be doing with the child. She just followed the script.”
Ongoing supervision
Regardless of baseline ASD experience, the more coaching supervision ECD practitioners had, the more comfortable they were in their new coaching role. Both ECD practitioners supported this sentiment:
“I’ve never engaged in something like this. I can actually see how I grew. I can actually see how I empowered this parent and through the parent, I can empower the child.”
An ESDM therapist commented: “It becomes more natural as they get more familiar with the intervention and the structure of the sessions.”
Positive coaching experience
A positive coaching experience was facilitated by a clear coaching structure and strong team relationships.
Caregiver coaching structure
The session plan, which outlined the content of each session in simple language, was found to be valuable:
“I think the coaching session, the paper that they always give to the ECD practitioner. I could see that every week they were adapted just to make it easier.”
“What worked was just repetition. Repetition of having a clear structure, clear instructions on what she needed to focus on, and then sticking as closely to the content of the coaching structure as we could.”
Due to this structure, participants reported understanding their roles. One ECD practitioner shared:
“My role is as a coach. My role is to empower the parent, so that the parent can help their child learn new skills. The parent goes back home and implements, then comes back to the sessions and I can see whether the parent took the skills, and went back home and practised those skills with their child.”
Strong team relationships
ECD school supervisors reflected on the good team relationships and how this created a platform for learning:
“What’s working is the relationship between everybody. Everybody plays a very big role. If we don’t have a relationship amongst each other, and the trust to ask questions, we wouldn’t be able to go forward.”
One of the ESDM therapists noted that they had, “good enough relationships” which were “flexible”. Another school supervisor commented:
“It’s been really good. The coach likes the ESDM therapists. They are very subtle when they coach the ECD practitioner to coach the mother. With maybe a touch or eye contact.”
Clear illustration of intervention concepts from session videos
Illustration of intervention skills
All participants found the videos “beneficial” to the implementation process, as the videos provided “visual” practical examples for caregivers and ECD practitioners. One of the ECD school supervisors said, “I don’t think we can do the coaching without the videos.” An ECD practitioner stated:
“The video is very beneficial. It’s a reminder for me of what I’ve learned in my training and what to coach on.”
One ECD school supervisor commented:
“I think the video brings more understanding to the parent. I think it gives you more confidence because you see a picture of what you supposed to do.”
Caregivers found that the videos helped them understand intervention concepts:
“The videos show you that when the child is interested in one thing, how to position yourself to be in the child’s eye line to get his attention.”
“When I watch the videos, I understand they’re giving choices and the parents are allowing the child to take the lead.”
Barriers to implementation
Barriers to implement caregiver coaching included: (I) complexity of some intervention and coaching concepts; (II) logistical challenges in the school setting; and (III) misalignment of video content with the South African context.
Intervention and coaching concepts
Participants described challenges related to the complexity of intervention and coaching concepts, and misalignment of caregiver coaching with ECD practitioner training in South Africa.
Complexity of concepts
All the participants expressed some difficulty with understanding intervention concepts, but the ESDM therapists, ECD practitioners and supervisors described some intervention concepts as “jargon:”
“Some of the language has a fair bit of jargon in it. Like a ‘joint activity routine.’ Even though it’s really nicely explained and set up, as a professional it’s much easier for me to understand. I hear it and I know what it refers to. I’m not always sure as a parent it would be that simple.”
South Africa is a multi-lingual nation. Therefore, ECD practitioners’ and caregivers primary language may not be English. An ECD supervisor stated:
“We have parents in our school that don’t understand English. That is a barrier to their understanding of their child’s diagnosis and what we are doing in the school.”
Misalignment of ECD practitioner training with a caregiver coaching approach
Collaborative coaching is a new concept for ECD practitioners:
“It was a big mind shift for ECD practitioners. In South Africa, if you’re a teacher you instruct the kiddos to do what you tell them to do. I think they were surprised by things that we didn’t seem as focused on.”
Certified ESDM therapists noted that “reflection” was particularly difficult for the ECD practitioners:
“I think around reflection, and picking up on cues from the parents, and how to balance sticking to a ‘script’ and listening to what parents say.”
An ECD practitioner commented:
“The beginning was very difficult because when we have to do reflections with the parent, there’re so many things happening in that moment, that the parent couldn’t remember what the child did, or I couldn’t remember.”
Logistical challenges
Logistical challenges in the school setting where caregiver coaching occurred, included time constraints and access to physical resources.
Time constraints
Participants reported time pressure, as they tried to fit caregiver coaching into their daily schedule. An ECD school supervisor described:
“It was a bit difficult because you teach. I have got my own class. There is a lot of potential. I think it can work, but it’s difficult for us to get out of the class.”
The ESDM therapists noted that the coaching put some strain on the ECD practitioners and their school supervisors.
“The Head of Department had to take time out of their schedule in order to be there. I would imagine that they were having to give an hour and a half per week to us.”
Access to physical resources
Access to dedicated coaching space, as well as a computer and the internet were potential implementation barriers. One of the ESDM therapists stated:
“What might impact at X school is the space that we have to work in. I think it’s a storage room.”
An ECD school supervisor however noted that they were making their space work for coaching:
“This is working at the moment. This small space that they are actually in. We have a baby monitor. We have got it all.”
Other logistical issues that impacted on coaching included access to a laptop to show the videos, and reliable internet.
“The buffering of the videos, it takes forever, and there is not enough bandwidth.”
Video content misaligned with South African context
Mismatch of material with the South African context
An ECD practitioner reflected:
“I had thoughts that these are not our communities, that is not how our communities operate, and those are not the type of homes that our kids come from.”
An ESDM therapist noted:
“I think it’s not nice to show parents something that they can’t afford. Because they start thinking, I need to have that in order to be able to do this. When in fact, the material is not the primary thing. They are a means to an end.”
One of the ECD school supervisors noted that she did not want caregivers to think they needed to have “this room, lounge or TV room” to use the skills at home.
Interestingly, caregivers did not indicate that video content was problematic:
“Generally it doesn’t matter whether it’s in the USA or whatever; kids are all the same.”
“Whenever you switch on the TV there’s only Americans anyway.”
Participants felt that South African videos would be of great value:
“I’d like to see us develop our own materials. I think that’s going to be more useful. Not all kids have those expensive toys. We need to be able to get parents to work with things they have.”
“We could reach more people if we talk the language of the country. Maybe English and Xhosa is not a bad idea if you want to target South Africans.”
Facilitators to sustain the intervention
Facilitators to sustain caregiver coaching included: (I) promising child and caregiver outcomes; and (II) structural factors including ongoing supervision and changes in the school system.
Child and caregiver outcomes
Participants were optimistic about child and caregiver outcomes they attributed to the coaching intervention.
Child outcomes
One caregiver reported improvements in his child’s language abilities:
“His speech has improved tremendously. He’s probably up to more than a hundred, 200 words, 4-word sentences.”
The other caregiver noted that her child was “showing affection,” having “fewer meltdowns,” his behavior had become “more manageable,” and he had begun to play with his siblings:
“I find that he still keeps his distance but he will engage with his sister, he will engage in her imaginary play as well.”
The ECD school supervisors also indicated “a lot” of child changes:
“I’ve seen the boy talking more, saying single words more, requesting, verbalizing his frustrations, “no” or “help”, “don’t want”, requesting, making choices, playing with mom, making eye contact with mom, inviting mom to play along. I’ve seen it first-hand.”
The ECD practitioners echoed similar reflections:
“I could see he’s starting to pick up words, even sentences. He’s gesturing with his whole body, and he makes eye contact with his mother. He’s just growing, just developing all of these skills through these sessions.”
An ESDM therapist noted:
“We‘ve been able to see more language, being able to stay in activities for longer, and definitely more communicative intent with his father.”
Caregiver ‘buy-in’
ESDM therapists felt the caregivers were “very invested” and “engaged”:
“The Dad is really committed, and is keen to keep on coming. He watches all the videos and he comes back and he’s got questions.”
An ECD school supervisor noted that the mother was:
“Doing her bit, she’s understanding the skills, making them her own, practising at home.”
A caregiver noted factors that maintained her interest in coaching:
“It doesn’t really affect your time commitment that much. We incorporate when he gets dressed, brushes his teeth, puts on his shoes, plays outside.”
The other caregiver noted:
“When we walk to the mall, there’s a big ToysRUs sign. The ToysRUs sign is red, orange, green, blue. That’s the way we taught him colors. Every day we walk past it, I go “red”, now he goes “red”, and now I go “yellow”, he goes “yellow”, “blue” and there’s another “blue”. It didn’t take any time because we walk past it every day.”
Caregiver competence
Caregivers reported:
“It’s given me confidence to say I can do it, I can help my son. Sometimes parents feel alone and they don’t know what they can do for their child.”
“The challenging part of having a special needs child is that you are not in control. When you as a parent do not know how to help, that makes you feel helpless. So, when you’ve been given a tool to help them, you feel empowered.”
An ECD practitioner described:
“Some of the parents don’t know how to deal with their children. Some of them lose hope. Some of them are frustrated. If they can come to this session, at least they will know how to deal with their children.”
One ECD school supervisor added: “I think this training boosts them.”
Structural factors promoting intervention sustainability
Ongoing supervision and structural changes to the school system could sustain caregiver coaching.
Ongoing supervision
In order to sustain caregiver coaching, ongoing supervision would be required. An ESDM therapist explained:
“As we go along the ECD practitioners develop more skills. I don’t think we should let them at this point work on their own without supervision.”
An ECD school supervisor commented:
“We will continue using the therapy when the study is over, but I’m just scared that the model won’t be implemented correctly.”
An ECD practitioner describes her supervision experience:
“The team really supported me where I needed support. They try to break it down and make it as simple as possible for me, so I can understand what I’m supposed to coach on.”
Feasibility within the school system
In order to sustain caregiver coaching, system-level factors need to be considered. An ESDM therapist reflected:
“If you want to give the ECD practitioner a bigger load… I do wonder how it’s going to happen if they already have a relatively full day?”
“It could be sustainable if the coach was freed from other duties so they can coach different parents. At the moment, they do that in addition to other tasks.”
One ECD practitioner noted:
“Most of the time when I was doing the session I had to leave my children to the assistants. It’s not fair because I have to be there for my children.”
An ECD school supervisor felt that it would be necessary to match caregiver coaching with parts of the school most closely aligned with outreach to caregivers:
“The main focus should rather be on X because she’s working with the home program.”
Barriers to sustain the intervention
Barriers included structural issues of poverty, lack of reliable transport, and unemployment.
Poverty, transportation, unemployment
One ESDM therapist shared:
“And what didn’t work? I think it is the intrusion of reality. The contextual factors. People are poor, and there is not great transport. We thought about them, and we knew that it’s a thing we have to consider. The one child can come because the father is unemployed. I think they have more resources than this other family. So the lesson to learn here, is for us to really think how we are going to work with these families in South Africa?”
The ECD practitioner described:
“The children that are at our school, they actually come from a very low socio-economic, poverty-stricken families.”
Discussion
This qualitative process evaluation investigated perceived barriers and facilitators to implement and sustain a non-specialist delivered, ESDM-informed caregiver coaching intervention in South Africa. Implementation facilitators included: (I) ongoing supervision and a clear session structure; (II) a positive coaching experience, which participants attributed to the coaching structure and strong team relationships; and (III) “Help is in your hands” ESDM video materials (Rogers SJ, Vismara L, Dawson G, et al. Help Is in Your Hands: A Web-Based Tool to Help Parents Build Their Toddlers’ Social and Communication Development 2017.).
Implementation barriers were reported either by one participant group (for example, only ECD practitioners), or were only experienced at the beginning of the implementation process. Implementation barriers included; (I) difficulty understanding some “complex” intervention concepts; (II) misalignment of ECD practitioner training with caregiver coaching, a barrier mitigated by ongoing supervision; (III) lack of space to conduct coaching sessions, which suggest that not all schools may be able to accommodate caregiver coaching without extra financial support and appropriate facilities; (IV) lack of consistent internet access. To work around this implementation barrier, the team downloaded videos to school computers and provided caregivers with a flash drive of video material. Limited access to the internet and the cost of data in LMICs is an important consideration when designing and implementing early ASD interventions in such settings (43); and (V) American videos in English. The utility of local adaptation of intervention materials is well documented (44-47). This will require local financial investment. In addition, South Africa is a multicultural, multilingual nation (48), therefore decisions to prioritize South African languages will need to be made. Importantly, even though the video material was American, all participants identified video content as contributing positively to caregiver coaching knowledge and skill.
Factors sustaining the intervention, included: (I) perceived improvements in child social communication abilities and caregiver factors such as “buy-in” and increased sense of competence; and (II) on-going supervision and support. While utilizing a non-specialist workforce for caregiver coaching may help address the capacity barrier in low resource environments (21); it is equally important to build specialist capacity in low resource settings. In South Africa ECD practitioners are expected to carry out their role under supervision and with the support of specifically designed programs. This is clearly specified in the National Integrated Early Childhood Development Policy (37). Therefore, to make any evidence-based early intervention sustainable, capacity building of both a non-specialist and specialist, supervisory workforce should occur.
Finally, the “intrusion of reality” was noted to be a barrier to sustain a caregiver coaching intervention in South Africa. This includes factors such poverty, lack of transportation, and limited access to health and education services. These contextual factors are particularly relevant in this part of the world, where socio-economic challenges continue to impact caregivers’ ability to access services (30).
This qualitative process evaluation highlights key implementation barriers and facilitators of a non-specialist-delivered, caregiver coaching early ASD intervention in South Africa. It also provides information on the outer setting, inner setting, and individuals involved in intervention implementation, delineated by the Consolidated Framework for Implementation Research (CFIR) (36), that will allow for further tailoring of the intervention approach to enhance contextual ‘fit’.
While early ASD intervention may align with Education Department goals and priorities, a shift in institutional support would need to occur to make this a sustainable approach, because the Education Department does not typically provide services for children younger than 7 years (26). Such a shift in institutional support could ensure dedicated ECD practitioner and supervisor time and resources to coach caregivers within the school setting.
Conclusions
This research forms part of a larger pilot study to improve access to early interventions for ASD in Africa (49). The findings highlight several pertinent facilitators and barriers for further exploration. Results will inform tailoring of the intervention training and supervision approach for the larger pilot study. Larger contextual and system-level issues such as poverty, the need for ongoing supervision, and local coaching materials in South African languages could offset potential positive child and caregiver outcomes.
Table S1
| A. Questions for caregivers who receive the intervention |
| i. What was your experience of the therapy? |
| ii. What worked and what didn’t work with the therapy? |
| iii. What outcomes did you see or are you seeing in your child? |
| iv. How did the therapy affect your time commitments at home? |
| v. Was it easy or difficult to include therapy in your daily schedule? |
| vi. Can you think of any changes or improvements we can make to the therapy that would make it easier for you to use in your home? |
| vii. Will you be able to continue using the therapy with your child when the project is finished? Why or why not? |
| viii. What was your experience of the videos? |
| ix. What worked and what didn’t work with the videos? |
| x. Can you think of any changes or improvements we can make to the videos? |
| xi. Did the fact that these were American families and children in the videos affect how you felt about the videos? |
| B. Question for early childhood development practitioners who deliver the intervention |
| i. How did the therapy work in your school? |
| ii. What worked and what didn’t work? |
| iii. How did it affect your workload, burden and space? |
| iv. What do you and others in your school think about the therapy, and how has that changed over time? |
| v. What outcomes did you see in the children you are working with? |
| vi. What changes should we make to the therapy or the training? |
| vii. Do you think you will continue using the therapy when the study is over? Why or why not? |
| viii. What was your experience of the videos? |
| ix. What worked and what didn’t work with the videos? |
| x. Can you think of any changes or improvements we can make to the videos? |
| xi. Did the fact that these were American families and children in the videos affect how you felt about the videos? |
| C. Questions for school supervisors of early childhood development practitioners |
| i. How did the therapy work in your school? |
| ii. What worked and what didn’t work? |
| iii. How did the therapy affect workload, burden, and space? |
| iv. What do you and others in your school think about the therapy, and how has that changed over time? |
| v. What outcomes did you see in the children the ECD practitioners are working with? |
| vi. What changes should be made to the therapy or training? |
| vii. Do you think your school will continue using the therapy when the study is over? Why or why not? |
| viii. What was your experience of the videos? |
| ix. What worked and what didn’t work with the videos? |
| x. Can you think of any changes or improvements we can make to the videos? |
| xi. Did the fact that these were American families and children in the videos affect how you felt about the videos? |
| D. Questions for certified Early Start Denver Model therapists who provide the training and supervision |
| i. How did ESDM operate in the schools? |
| ii. What worked and what didn’t work? |
| iii. How did ESDM affect workload, burden and space in the schools? |
| iv. How was ESDM received by those who worked with it in the schools, and how did that change over time? |
| v. What outcomes did you see or are you seeing in the children? |
| vi. Was there feedback and what was it?/What feedback did you obtain? |
| vii. What changes should be made to the ESDM training you led, the supervision you are providing, or the session structure? |
| viii. Do you see think ESDM would be sustainable in the school setting? |
| ix. What was your experience of the videos? |
| x. What worked and what didn’t work with the videos? |
| xi. Can you think of any changes or improvements we can make to the videos? |
| xii. Did the fact that these were American families and children in the videos affect how you felt about the videos? |
ESDM, Early Start Denver Model; ECD, Early Childhood Development.
Acknowledgments
Funding: This work was supported by the National Institutes of Mental Health (K01-MH-104370 to L Franz), the Duke Global Health Institute (to L Franz), the National Research Foundation (to PJ de Vries), the University of Cape Town Programme for Enhancement of Research Capacity (to PJ de Vries), and the Struengmann Fund (to PJ de Vries).
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Pediatric Medicine for the series “Implementing Autism Early Intervention: A Global Perspective”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/pm.2019.07.08). The series “Implementing Autism Early Intervention: A Global Perspective” was commissioned by the editorial office without any funding or sponsorship. LF serves as an unpaid Guest Editor of this series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical clearance was obtained from the University of Cape Town (HREC 039/2015), Duke University (IRB Pro00064533), and the Western Cape Education Department. Informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Elsabbagh M, Divan G, Koh YJ, et al. Global Prevalence of Autism and Other Pervasive Developmental Disorders. Autism Res 2012;5:160-79. [Crossref] [PubMed]
- Franz L, Chambers N, von Isenburg M, et al. Autism Spectrum Disorder in Sub-Saharan Africa: A Comprehensive Scoping Review. Autism Res 2017;10:723-49. [Crossref] [PubMed]
- World Bank. Sub-Saharan Africa 2018 [March 7, 2018]. Available online: https://data.worldbank.org/region/sub-saharan-africa?view=chart
- Kieling C, Baker-Henningham H, Belfer M, et al. Child and adolescent mental health worldwide: evidence for action. Lancet 2011;378:1515-25. [Crossref] [PubMed]
- Global Research on Developmental Disabilities Collaborators. Developmental disabilities among children younger than 5 years in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Global Health 2018;6:e1100-e1121. [Crossref] [PubMed]
- Weitlauf AS, McPheeters ML, Peters B, et al. AHRQ Comparative Effectiveness Reviews. Therapies for Children With Autism Spectrum Disorder: Behavioral Interventions Update 2014. PubMed PMID: 25210724. Available online: https://www.ncbi.nlm.nih.gov/books/NBK241444/
- Warren Z, McPheeters ML, Sathe N, et al. A Systematic Review of Early Intensive Intervention for Autism Spectrum Disorders. Pediatrics 2011;127:e1303-e1311. [Crossref] [PubMed]
- Strauss K, Mancini F, Fava L. Parent inclusion in early intensive behavior interventions for young children with ASD: A synthesis of meta-analyses from 2009 to 2011. Res Dev Disabil 2013;34:2967-85. [Crossref] [PubMed]
- Reichow B. Overview of Meta-Analyses on Early Intensive Behavioral Intervention for Young Children with Autism Spectrum Disorders. J Autism Dev Disord 2012;42:512-20. [Crossref] [PubMed]
- Peters-Scheffer N, Didden R, Korzilius H, et al. Cost comparison of early intensive behavioral intervention and treatment as usual for children with autism spectrum disorder in the Netherlands. Res Dev Disabil 2012;33:1763-72. [Crossref] [PubMed]
- Eldevik S, Hastings RP, Hughes JC, et al. Meta-Analysis of Early Intensive Behavioral Intervention for Children With Autism. J Clin Child Adolesc Psychol 2009;38:439-50. [Crossref] [PubMed]
- World Health Organisation. Caregiver skills training for the management of developmental disorders 2015 [cited 2018]. Available online: http://www.who.int/mental_health/mhgap/evidence/resource/child_q6.pdf?ua=1
- Ruparelia K, Abubakar A, Badoe E, et al. Autism Spectrum Disorders in Africa: Current Challenges in Identification, Assessment, and Treatment: A Report on the International Child Neurology Association Meeting on ASD in Africa, Ghana, April 3-5, 2014. J Child Neurol 2016;31:1018-26. [Crossref] [PubMed]
- Morris J, Belfer M, Daniels A, et al. Treated prevalence of and mental health services received by children and adolescents in 42 low-and-middle-income countries. J Child Psychol Psychiatry 2011;52:1239-46. [Crossref] [PubMed]
- de Vries PJ. Thinking globally to meet local needs: autism spectrum disorders in Africa and other low-resource environments. Curr Opin Neurol 2016;29:130-6. [Crossref] [PubMed]
- Reichow B, Servili C, Yasamy MT, et al. Non-Specialist Psychosocial Interventions for Children and Adolescents with Intellectual Disability or Lower-Functioning Autism Spectrum Disorders: A Systematic Review. PLoS Med 2013;10:e1001572 [Crossref] [PubMed]
- Wong VC, Kwan QK. Randomized Controlled Trial for Early Intervention for Autism: A Pilot Study of the Autism 1-2-3 Project. J Autism Dev Disord 2010;40:677-88. [Crossref] [PubMed]
- Tsang SK, Shek DT, Lam LL, et al. Brief Report: Application of the TEACCH Program on Chinese Pre-School Children with Autism--Does Culture Make a Difference? J Autism Dev Disord 2007;37:390-6. [Crossref] [PubMed]
- Zhou B, Xu Q, Li H, et al. Effects of Parent-Implemented Early Start Denver Model Intervention on Chinese Toddlers with Autism Spectrum Disorder: A Non-Randomized Controlled Trial. Autism Res 2018;11:654-66. [Crossref] [PubMed]
- Rahman A, Divan G, Hamdani SU, et al. Effectiveness of the parent-mediated intervention for children with autism spectrum disorder in south Asia in India and Pakistan (PASS): a randomised controlled trial. Lancet Psychiatry 2016;3:128-36. [Crossref] [PubMed]
- Divan G, Vajaratkar V, Cardozo P, et al. The Feasibility and Effectiveness of PASS Plus, A Lay Health Worker Delivered Comprehensive Intervention for Autism Spectrum Disorders: Pilot RCT in a Rural Low and Middle Income Country Setting. Autism Res 2019;12:328-39. [Crossref] [PubMed]
- Schreibman L, Dawson G, Stahmer AC, et al. Naturalistic Developmental Behavioral Interventions: Empirically Validated Treatments for Autism Spectrum Disorder. J Autism Dev Disord 2015;45:2411-28. [Crossref] [PubMed]
- Guler J, de Vries PJ, Seris N, et al. The importance of context in early autism intervention: A qualitative South African study. Autism 2018;22:1005-17. [Crossref] [PubMed]
- World Bank. Data for Sub-Saharan Africa, South Africa 2019 [March 28, 2019]. Available online: https://data.worldbank.org/?locations=ZG-ZA
- Sulla V, Zikhali P. Overcoming poverty and inequality in South Africa: An assessment of drivers, constraints and opportunities. Washington, DC: The World Bank Group, 2018.
- Franz L, Adewumi K, Chambers N, et al. Providing early detection and early intervention for autism spectrum disorder in South Africa: stakeholder perspectives from the Western Cape province. J Child Adolesc Ment Health 2018;30:149-65. [Crossref] [PubMed]
- Statistics South Africa. Statistical Release: Gross Domestic Product. Statistics South Africa, 2017.
- van Schalkwyk GI, Beyer C, de Vries PJ. South Africa and Autism. In: Volkmar FR. editor. Encyclopedia of Autism Spectrum Disorders. New York, NY: Springer New York, 2015:1-7.
- Springer PE, van Toorn R, Laughton B, et al. Characteristics of children with pervasive developmental disorders attending a developmental clinic in the Western Cape Province, South Africa. South African Journal of Child Health 2013;7:95-9. [Crossref]
- Mayosi BM, Benatar SR. Health and Health Care in South Africa—20 years after Mandela. N Engl J Med 2014;371:1344-53. [Crossref] [PubMed]
- Khalfani AK, Zuberi T. Racial classification and the modern census in South Africa, 1911-1996. Race and Society 2001;4:161-76. [Crossref]
- Pillay S, Duncan M, de Vries PJ. How many children with Autism Spectrum Disorder are there in South African Schools: A systematic database search for known cases of ASD in the Western Cape. Poster presented at the Regional International Meeting for Autism Research (IMFAR) in Africa, and 19th Congress of the South African Association of Child & Adolescent Psychiatrists and Allied Professions (SA-ACAPAP) 2017, September.
- Chambers NJ, Dawson-Squibb JJ, Franz L, et al. African Autism Treatment Network (AATN): Lessons Learned. Poster presented at the SA-ACAPAP in Johannesburg South Africa 2019, May.
- Dawson G, Rogers S, Munson J, et al. Randomized, Controlled Trial of an Intervention for Toddlers With Autism: The Early Start Denver Model. Pediatrics 2010;125:e17-e23. [Crossref] [PubMed]
- Ramseur K 2nd, de Vries PJ, Guler J, et al. Caregiver descriptions of joint activity routines with young children with autism spectrum disorder in South Africa. Pediatr Med 2019; [Crossref] [PubMed]
- Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4:50. [Crossref] [PubMed]
- Government of South Africa. National Integrated Early Childhood Development Policy. Pretoria: Government Printers, 2015.
- Curran GM, Sullivan G, Mendel P, et al. Implementation of the CALM intervention for anxiety disorders: a qualitative study. Implement Sci 2012;7:1-11. [Crossref] [PubMed]
- Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients‘ care. Lancet 2003;362:1225-30. [Crossref] [PubMed]
- Gagliardi AR, Alhabib S. members of Guidelines International Network Implementation Working Group. Trends in guideline implementation: a scoping systematic review. Implement Sci 2015;10:54. [Crossref] [PubMed]
- Fischer F, Lange K, Klose K, et al. Barriers and Strategies in Guideline Implementation—A Scoping Review. Healthcare 2016;4:1-16. [Crossref] [PubMed]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology 2006;3:77-101. [Crossref]
- Wetherston V, Gangat S, Shange N, et al. The views and knowledge of parents of children with autism spectrum disorder on a range of treatments. South African Journal of Child Health 2017;11:117-21. [Crossref]
- Harrison AJ, Long KA, Manji KP, et al. Development of a Brief Intervention to Improve Knowledge of Autism and Behavioral Strategies Among Parents in Tanzania. Intellect Dev Disabil 2016;54:187-201. [Crossref] [PubMed]
- Hampton LH, Harty M, Fuller EA, et al. Enhanced milieu teaching for children with autism spectrum disorder in South Africa. Int J Speech Lang Pathol 2019;1-11. [Epub ahead of print]. [Crossref] [PubMed]
- Cheremshynski C, Lucyshyn JM, Olson DL. Implementation of a Culturally Appropriate Positive Behavior Support Plan With a Japanese Mother of a Child With Autism: An Experimental and Qualitative Analysis. J Posit Behav Interv 2012;15:242-53. [Crossref]
- Chambers NJ, Wetherby AM, Stronach ST, et al. Early detection of autism spectrum disorder in young isiZulu-speaking children in South Africa. Autism 2017;21:518-26. [Crossref] [PubMed]
- Statistics South Africa. City of Cape Town - 2011 Census - Cape Town: Statistics South Africa,; 2012. Available online: http://resource.capetown.gov.za/documentcentre/Documents/Maps%20and%20statistics/City_Statistics_2012.pdf
- Franz L, Viljoen M, Seris N, et al. Pilot Study to Improve Access to Early Intervention for Autism in Africa. Poster presented at the 10th Anniversary Conference: Global Mental Health Research without Borders, in Bethesda, MD, USA 2019, April.
Cite this article as: Makombe CBT, Shabalala N, Viljoen M, Seris N, de Vries PJ, Franz L. Sustainable implementation of early intervention for autism spectrum disorder through caregiver coaching: South African perspectives on barriers and facilitators. Pediatr Med 2019;2:39.