Early screening and diagnosis for ASD children in China
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder that starts from the infantile period, which can be characterized by communication and social interaction deficits, limited interests, and stereotyped behavior (1). Dr. Leo Kanner first reported and proposed the concept of autism in 1943 (2). Since autism was treated as an independent disorder by DSM-III in 1980 and officially defined by the medical community, the prevalence of the disorder reported in various countries has increased gradually. Monitoring data published by Autism and Developmental Disabilities Monitoring Network (ADDM Network) over the past decade have shown that the prevalence of ASD increased from 0.67% (1/150) in 2000 to 1.69% (1/59 in 2014) (3). It is estimated that the global average prevalence rate of autism is about 1% (4). China is short of national epidemiological statistics of the disorder at present, and the reported prevalence of ASD varies significantly among regions from approximately 0.93 to 11.40/1,000 (5-7). Furthermore, a sample survey of disabled children in China shows that ASD is the leading cause of disability among disabled children under six years of age (8).
ASD is one of the fastest growing disabilities (9), which leads to a significant burden for families and society. The World Health Organization (WHO) points out that ASD has become a severe public health concern which affects the quality of life and the health of the population (10). According to a study from the United States, the annual financial cost associated with providing services and support for children with ASD is between $11.5 billion and $60.9 billion (11). Also, the average annual expenditure of children with ASD is 4.1–6.2 times higher than that of children without ASD (12). A survey conducted in Heilongjiang Province shows that the average total expenditure on rehabilitation for the family with ASD children is 64.4 thousand yuan per year ($9,571). While, 12.7% of total expenditure for rehabilitation in the family with ASD children is more than 100 thousand yuan ($14,862), among which 81.5% of families believe that the total expenditure of rehabilitation for children with ASD has resulted in an adverse influence on family economy. At the same point, rehabilitation and transportation accounted for the largest share of expenditure,followed by housing rental, consulting and medical treatment (13).
At present, the consensus of diagnosis and treatment for ASD achieved both in China and abroad is the importance of early detection and early intervention (14,15). In recent years, extensive studies support early identification and diagnosis of ASD and standardized behavioral therapy contribution to the improvement of the prognosis for ASD children, which could facilitate better integration into the society and reduction of the disease burden of the target population (16,17). ASD can be reliably diagnosed at about 2 years old (18), but in reality, the age at diagnosis of ASD children is generally older, with the average diagnostic age of ASD reported at present is about 4.5 years old in the United States (18), causing many children with ASD to lose the opportunity to receiving early intervention in the critical period. In order to solve this problem, various countries in Europe and the United States have carried out ASD early screening for children under three years of age (19-21). The American Academy of Pediatrics (AAP) recommends that all children aged 18–24 months should also receive ASD screening (22) during routine health check-up so that more ASD children can be identified and have the opportunities for early intervention at an early age.
Studies on ASD have been carried out in China for less than 40 years, with Professor Tao Guotai first reporting on ASD in 1982 (23). Although it is nearly 40 years later than the first international report, Chinese scholars have made remarkable achievements in the epidemiology, etiology, diagnosis, and treatment of ASD with the improvement of awareness amongst medical professionals and medical level. Here, a review of the related research on early screening and diagnosis of ASD in China has been performed.
Early screening and diagnostic tools for ASD children in China
Recognition of early signs in ASD
Social interaction difficulties and partial stereotypes of ASD will appear at an early age, and early screening is aimed at these behavioral abnormalities (24). Accordingly, the Expert Consensus on Early Identification Screening and Intervention for Children with ASD (15) was compiled for the first time by discussions of the Developmental Behavior Group in the Pediatric Branch of the Chinese Medical Association and relative experts, combined with ASD research progress at home and abroad (14,24,25). Five behavioral markers for early recognition of ASD have been proposed, briefly called the “five no” behaviors:
- No (less) eye contact: refers to abnormal eye contact. ASD children will show a deficiency or decrease of visual attention stimulated by intentional social interaction in early childhood, especially decrease of visual attention on human eyes.
- No (fewer) response: includes name calling response and instructions response Children do not react to their parents’ calls and insensitive to their names, which can generally be one of the earliest ASD signs discovered by parents.
- No (less) pointing: refers to lack of proper body movements and joint attention. Children cannot express their needs and willingness through appropriate body movements, such as inability to nod to indicate their needs, shake head to indicate no, purposeful pointing, gesturing, etc. Joint attention refers to a coordinated attention ability in the early social cognitive development of children. It involves the process of coordinated visual attention between the two people on an object or event using finger pointing or eyesight.
- No (fewer) words: refers to a delay in speaking ability. This is often the primary concern of ASD parents. Expressive language delay is not a core diagnostic features for an ASD diagnosis because other developmental behavioral disorders also show such delays. Nevertheless, ASD may still be considered for children with expressive language delay in the clinic.
- Inappropriate behavior It indicates inappropriate use of objects and abnormalities related to perception, which include rotation, alignment, and continuous visual exploration of objects. For example, arranging cars in a row, rotating things and gazing at them always. Also, improper speech should also be a concern. This could represent a regression of speech after the appearance of ordinary language, as well as unintelligible, meaningless language, or repeating words or phrases of others.
In addition, in 2013, the National Health and Family Planning Commission of China compiled an early screening tool for children’s psychological and behavioral developmental problems at a basic level in China based on collected experiences of senior experts in the field of children’s psychology and development, called “Early Warning Signs of Children’s Psychological and Behavioral Development Problems” (26). It is composed of eight-time points in the age range of 0–3 years, and each time point contains four items. Any positive early warning sign in this age group may suggest the possibility of developmental deviation. The items at each time point contain warning signs of common abnormalities, including “no response for name calling”, “inability to point at people or things as required”, “no eye contact with people”, etc. Additionally, early warning signs can be assessed based on children’s behavior by medical professionals, parents, other caregivers, and teachers.
Other scholars have combined the early signs of ASD with the screening checklist in the early screening of ASD. For example, Li et al. carried out an initial screening investigation of ASD in children receiving routine physical examination in Xuhui District, Shanghai by using CHAT-23 checklist. Two early warning indicator tests of ASD, including response to name call, and instructions, performed by community child health physicians were added into the level-I screening group. Children would be defined as a partial positive of level-I screening when both tests were not passed. Eventually, the results showed that 8.11% of ASD children would be missed if they only use CHAT-23 without the two early warning indicator tests (27).
Therefore, China has relatively sophisticated tools, relatively perfect expert consensus, and practical research support in the field of recognition of early signs in ASD. In the future, prospective cohort studies can be conducted to investigate and explore the early signs of ASD children in China, which will provide more evidence for the early recognition of ASD.
Status of ASD screening scales
In the early screening and diagnosis of ASD, the tools used include level 1 screening tools, level 2 screening tools, and diagnostic tools. Level 1 screening tool is used to detect suspected ASD in the general population. Level 2 screening tools are applied to exclude other developmental disorders in high-risk ASD populations (such as a family history of related disorders, positive level 1 screening, etc.). Furthermore, ASD diagnosis mainly depends on clinical observation and parent report of child development in which diagnostic criteria primarily include the tenth revision of the International Classification of Diseases (ICD-10), the fifth edition of the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM-5) or the third edition of the Chinese Classification and Diagnostic Criteria for Mental Disorders (CCMD-3). Appropriate diagnostic tools can inform the final diagnosis during clinical observation and parent report. Here, the article summarizes the early screening and diagnostic tools of ASD introduced and used by Chinese scholars.
Level 1 screening tools
Modified Checklist for Autism in Toddlers (M-CHAT)
Checklist for Autism in Toddlers (CHAT)is the first tool used for ASD screening in toddlers that was compiled by the British scholar Bukin IuV in 1992 (28). Robins et al. modified the checklist in 2001, with the compiling of a new Modified Checklist for Autism in Toddlers (M-CHAT) (29), which became the most widely used ASD screening tool in recent years. However, Robins et al. revised the M-CHAT again in 2014, and published the latest Modified Checklist for Autism in Toddlers, Revised, with Follow-Up (M-CHAT-R/F) which is a 2-stage parent-report screening tool to assess risk for ASD (30). Subsequently, Chinese scholars, Gong et al. introduced and localized M-CHAT in Chinese, and published a revised version of M-CHAT in Chinese. Clinical application of the translated versions provided good overall validity and reliability results. The sensitivity was 0.96, and the specificity was 0.60 (31,32). Moreover, based on the above version, the author compiled a simplified version of M-CHAT in Chinese, eliminating five items that had shown poor validity or reliability in previous studies in the Chinese revision of the M-CHAT. As a result, the simplified version of the M-CHAT in Chinese is superior to that of the Chinese version of M-CHAT in the aspects of validity and reliability. When the cutoff point was set at 13, the sensitivity was 92%, and the specificity was 83%. The positive predictive value (PPV) and the negative predictive value (NPV) were 82.7% and 89.2%, respectively, therefore currently the simplest and most convenient version at present, and deserves to be widely applied in the screening of early autism in toddlers in China (33). Also, the Chinese version of M-CHAT-R/F has been revised by Jing et al., showing satisfactory reliability, validity, and cultural applicability, with corresponding data to be published (34).
Checklist for Autism in Toddlers-23 (CHAT-23)
This checklist was compiled by Virginia Wong et al. from the University of Hong Kong in 2004 (35). The CHAT-23 includes the parent-reported questions of the M-CHAT as section A (CHAT-23-A) and the observational part of the CHAT as section B (CHAT-23-B) which formed a new Chinese version of Autism Screening Checklist for toddlers at 18–24 months. Xu et al. introduced the checklist into mainland China and researched its reliability and validity. Results suggested that the sensitivity and specificity of CHAT-23 parental questionnaires were 0.941 and 0.884, and the checklist could be used as an early screening tool for ASD in primary medical institutions of maternal and child health care system in routine physical examination of healthy children (36). At present, CHAT-23 has been used as a screening tool in the routine physical examination screening network of ASD for toddlers in partial areas of Shanghai (27). The introduction of this checklist has promoted the development of early screening research for ASD in China.
Clancy Autism Behavior Rating Checklist (CABRS)
Professor Clancy compiled this checklist in 1968 (37). There are 14 items in CABRS, screen positive is considered a total score of ≥7. The checklist should be filled in by parents, which is suitable for rapid ASD screening (38) of children aged 2 to 15 years in pediatric clinics, kindergartens, and schools. Ke et al. researched the reliability and validity of the checklist in 2002, the CABRS was tested in 52 cases of ASD children and 48 non-ASD controls. The scores of the ASD patient (18.90±3.32) were markedly higher than that of the controls. With the exception of item 4, there were significant differences in the scores of the other 13 items (39). This edition is currently widely used in China in an epidemiological investigation and ASD evaluations (40). Despite a wide application of this version, it has not been updated since it was compiled. Accuracy of this checklist could be improved by aligning it with updated ASD diagnostic criteria.
Autism Spectrum Rating Scale (ASRS)
The questionnaire was compiled by Dr. Goldstein and Dr. Naglieri in 2009, including the full version and the simplified version of the Autism Spectrum Rating Scale (ASRS) (41). The full version has 71 items, and the latter contains 15 items. Parents or teachers can complete each version. It is suitable for ASD screening in children aged 2–5 and 6–18 years (41). In 2013, Chinese scholar Zhou et al. conducted a Chinese study of the ASRS, where they established local norms. The study shows that the internal consistency ranged from 0.585 to 0.929 and suggested a cutoff ≥60 for the Chinese version of the ASRS, with good accuracy in screening autism symptoms (sensitivity =94.2%, specificity =77%). ASRS was the first ASD screening tool to be revised and normed in China. ASRS has been used as a screening tool for multi-center epidemiological studies of ASD in children in China (42-45).
Screening Checklist for Childhood Autism
The checklist was compiled by Chinese scholar Liu et al. in 2004. Three key components of the ASD profile were chosen to focus on for the checklist. A total of 17 items were included: 7 items on social interaction, six items on speech and communication, and four items on interests and behaviors. The checklist had satisfactory reliability including good inter-rater reliability (0.933), test-retest reliability (0.986), split-half reliability (0.969). There were significant differences in the total scores of the checklist between the ASD group and intellectual disability group, ASD group, and typically developing group (P<0.01) (46). Compared with other commonly used autism screening checklists (such as M-CHAT, ASRS), this checklist has fewer items and shorter filling time, which make it a popular screening tool amongst clinicians. However, the author of the checklist also believes that the reliability or validity of some of the individual items of the checklist is poor, so it should be further revised. The validity of the scale should be further studied when it is applied to the general population and atypical or high-functioning ASD (46).
Level 2 screening tools
Autism Behavior Checklist (ABC)
The checklist was compiled by Krug et al. in the 1980s. It is a 4-point Likert scale contains a total of 57 items, including five dimensions of feeling, behavior, language, movement, and communication. The highest score of the checklist is 158. The ABC is suitable for ASD screening among people aged 3–35 years (47). The Chinese version of ABC was first reported in 1993 and was introduced by Yang et al. (48). It was widely used for assisted diagnosis, epidemiological investigation, and evaluation of intervention effects of ASD in China (49,50). While ASD diagnostic criteria as people's awareness of ASD have changed in recent years, the scale has not been revised since it was established. Also, there is a study that has found that ABC cannot distinguish ASD from other developmental disorders accurately (51). Therefore, the use of this checklist in subsequent ASD research in China is questionable.
Social Communication Questionnaire (SCQ)
Rutter and Lord compiled this questionnaire in 1999 based on the ASD diagnostic standardized tool, the Autism Diagnostic Interview-Revised (ADI-R) (52). The questionnaire consists of 40 items and three dimensions: social communication, communication, and repetitive, stereotyped behavior. Total score ≥15 indicates positive primary screening. This questionnaire applies to the screening of ASD for children with the mental age of >2 years (52). The Chinese version of SCQ was introduced by Xu et al. in 2009. The reliability and validity of the questionnaire were investigated by enrolling 867 children aged 2–6 years old in kindergarten (53). The total score of SCQ was normally distributed, suggesting the limited ability of the SCQ to distinguish children with ASD from those without ASD in China. These results suggested that SCQ might not be appropriate as a primary screening tool for ASD in China, but it may be acceptable when combined with other questionnaires to be a secondary screening tool (53).
Status of ASD Diagnostic Instruments
Child Autism Rating checklist (CARS)
The CARS was compiled by Schopler et al. in 1988 and included 15 items. Each CARS domain is scored on a scale ranging from one to four (54). Children may be defined as non-ASD, moderate ASD or severe ASD when the total score is <30, between 30 to 36, and >36, respectively. This checklist is suitable for people beyond two years old (54). In 2004, Li et al. researched the reliability and validity of the Chinese version of CARS (55). The sensitivity and specificity of the checklist were reported by the authors to be 100% when 30 points were used as the critical diagnostic value, indicating a high diagnostic efficiency (55) (Cautionary statement: It is impossible for specificity and sensitivity to be both 100%, it may be due to the sample in their study was very distinct, but the author did not mention that.). At present, the checklist is the most widely used diagnostic auxiliary tool for ASD in China.
Autism Diagnostic Observation Schedule, Second Edition (ADOS-2)
The ADOS-2 is a semi-structured, standardized assessment of social interaction, communication, play, imaginative use of materials, and restricted and repetitive behaviors (56). The ADOS was compiled in the early 1990s and has been revised several times, most recently in 2006. The ADOS-2 is divided into five modules based on the expressive language ability of the participant (56,57). The ADOS-2 has not been formally introduced in mainland China and has not been widely applied in China despite its broad application in Western countries. At present, the ADOS-2 used in mainland China is the traditional Chinese version in Taiwan, China. Zhou et al. have investigated the reliability and validity of ADOS-2 module 1, the results showed that the Cronbach’s α coefficient of the entire schedule was 0.93. Moreover, according to the DSM-V criteria, the consistency rate of the clinical diagnoses and ADOS classifications was 91.1%. The sensitivity and specificity of ADOS-Module 1 was 96.5% and 61.5%, respectively, suggesting it could be widely used as a tool to help inform ASD diagnosis in China (58). However, reliably administering the ADOS-2 requires evaluators to have specific qualifications. Also, administration and scoring can take between 1–1.5 hours, and may, therefore, be more applicable for diagnostic quality control in major epidemiological studies of ASD than clinical practice.
Autism Diagnostic Interview-Revised (ADI-R)
The ADI-R is a standardized, semi-structured clinical interview, developed in the 1980s, widely used in clinical practice and research, and alongside the ADOS-2 is considered a ‘gold standard’ tool to inform ASD diagnosis in Western countries (59). The interview ought to be led by clinical personnel who have been formally trained in the ADI-R and obtained international certification. Parents (or the primary caregivers) report on participants who are beyond the mental age of 2 years and provide the physicians with the details of their children’s specific behaviors, rather than the general judgment of each reported problem. Finally, the key to scoring depends on the accuracy of the information provided (59). The only authorized Chinese version of the ADI-R and its guidance manual is the traditional Chinese version translated by Taiwan, China. In 2002, Guo et al. in the Institute of Mental Health, Peking University, conducted a reliability and validity study on the simplified Chinese version of ADI-R with 50 children with ASD, the results showed that in the diagnostic validity study, all but one item (B46: friendship with fellows)of the 16 reciprocal social interaction items showed significance for differential diagnosis of autism (P<0.01).Moreover, so did 11of 13 communication and language items and 4 of 8 restricted, stereotyped behaviors items (P<0.01). In the reliability study, the kappa between interviewers for 15 of the 16 reciprocal social interaction items, for 10 of the 13 communication and language items and 3 of the 8 restricted, stereotyped behaviors items exceeded 0.677. Moreover, the study concluded that the ADI-R presented good diagnostic validity and high reliability (60). However, up to now, this version has not been officially published, with relatively limited clinical application. Similar to the ADOS-2, the ADI-R has high requirements for the qualification of evaluators and the duration of the evaluation is long (2–2.5 hours for ADI-R). At present, the ADI-R is mostly used for quality control in scientific research projects in China.
In conclusion, numerous ASD screening and diagnostic tools have been introduced and localized by Chinese scholars. However, few have been updated and improved, and there is only one set of ASD assessment tools (Screening Checklist for Childhood Autism) developed for children based on their Chinese cultural background. Future research should attempt to adapt ASD screening and diagnostic tools further and develop more suitable ASD screening and diagnostic tools for people of Chinese cultural backgrounds.
Current situation of ASD early screening in China
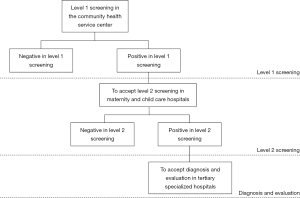
In China, a three-level child healthcare system has been established: community health service centers act as the first level; district maternity and child healthcare hospitals act as the second level, and municipal maternity and children’s healthcare/children’s hospitals (tertiary hospitals) act as the third level. These institutions provide essential health services and monitoring to children aged 0 to 6 years. Routine services include growth and development assessments, newborn screening, nutrition and feeding guidance, hearing and vision screening, and neuropsychological development evaluations. Primary care pediatricians and healthcare professionals in the first and second level child health system are responsible for screening, monitoring, and referral, while pediatricians at the third level child healthcare system are responsible for the diagnosis, consultation, and treatment (61).
Most researchers will rely on the third-level child health care system and adopt the two-level screening plus two-level referral model in the early screening of ASD. All children who have routine health check-ups in the community health service centers are the screening target. The primary screening process is as follows: the medical provider provides the level 1 screening tools (such as CHAT-23-A) at the level 1 screening, and the child’s caregiver completes it. Level 1 screen-positive children are referred to secondary hospitals/maternity and child care hospitals for level 2 screening (such as CHAT-23-B). Children with positive level 2 screening are referred to the tertiary specialized hospitals/public hospitals for evaluation and diagnosis. A detailed flow process the three-level child healthcare system is shown in Figure 1.
Li et al. provided several improvements to the necessary screening process, such as an added observational component in level 1 screening; telephone follow-ups with the screen-positive families; and dissemination of information on ASD to families. The results of their study indicated that the screen-positive rate and the slow rate of referral for level 1 screening were significantly improved (27). In other studies with smaller sample sizes, level 2 screening was omitted or carried out simultaneously with the diagnostic evaluation (53,62). These studies reported a reduction in the loss to follow-up during Level 2 referral, but because of the heavy workload of Level 2 screening, this approach is not applicable in researches of large sample size. Other researchers conducted cross-sectional studies which aimed to determine the prevalence and explore the application of screening tools in the early screening of ASD (63,64). Children in local jurisdictions were selected using stratified cluster sampling for level 1 and level 2 screening, and diagnostic evaluation (63,64). However, this method can only be used to determine the prevalence of ASD in the area and does not apply for the screening of all children. The first study on early screening of ASD in China was conducted by Huang et al. in Tianjin in 2009 (64). The study was cross-sectional and involved 8,424 children aged 18–30 months, with final ASD diagnostic rate of 2.7‰. Subsequently, studies of early screening and diagnosis of ASD have been conducted by scholars in Shanghai, Shenzhen, Lianyungang, and other places (53,62-69). Most of the screening ages were 18–24 months, and the final diagnosis rate of ASD ranged from 0.82–11.4‰. Table 1 indicates early screening and early diagnostic studies of ASD in various regions of China. Study ASD prevalence rates vary significantly in different areas, which may be related to different screening tools, diagnostic tools, and screening management models used in various studies.
Table 1
| Time | Area | Sample size | Age, range | Screening instrument | Diagnostic criteria and instrument | Positive rate of screening | Diagnosis rate | |
|---|---|---|---|---|---|---|---|---|
| Level 1 | Level 2 | |||||||
| 2009 | Tianjin | 8,424 | 18–30 months | CHAT | NA | DSM-IV | NA | 2.7‰ |
| 2010 | Shanghai | 484 | 18–24 months | CHAT-23-A | CHAT-23-B | DSM-IV | 11.98% | 4.1‰ |
| 2011 | Shanghai | 867 | Preschool | SCQ | NA | DSM-IV | 7.2% | 2.3‰ |
| 2012 | Shenzhen | 3,624 | 18–24 months | CHAT | CARS | DSM-IV | 5.77% | 2.76‰ |
| 2012 | Lianyungang | 2,090 | 18–36 months | CHAT-23-A | CHAT-23-B, ABC, CARS | DSM-V | NA | 11.4‰ |
| 2012–2013 | Shanghai | 2,089 | 18–24 months | CHAT-23-A | CHAT-23-B | NA | 3.54% | 2.9‰ |
| 2012–2014 | Ningbo | 88,238 | <36 months | M-CHAT | ABC, CARS | DSM-V, ADI-R, ADOS-2 | 0.49% | 0.82‰ |
| 2013 | Shenzhen | 1,845 | 18–24 months | CSBS | NA | NA | 7.32% | NA |
| 2014–2017 | Shanghai | 22,247 | 18–24 months | CHAT-23-A | CHAT-23-B | DSM-V, ADI-R, ADOS | 3.26% | 3.2‰ |
CHAT-23-A, section A of Chinese-validated version of the Checklist for Autism in Toddlers; CHAT-23-B, section B of Chinese-validated version of the Checklist for Autism in Toddlers; SCQ, social communication questionnaire; CHAT, Checklist for Autism in Toddlers; M-CHAT-F, Modified Checklist for Autism in Toddlers with follow-up; CSBS, Communication and Symbolic behavior Scales; CARS, Child Autism Rating Scale; ABC, autism behavior checklist; DSM, Diagnostic and Statistical Manual of Mental Disorders; ADI-R, autism diagnostic interview-revised; ADOS-2, autism diagnostic observation schedule.
Early detection and diagnosis of ASD is a critical step to provide timely early intervention, which may improve the prognosis of ASD (17,70,71). Comparing children diagnosed with ASD, Huang et al. found that 58.1% of the children diagnosed with ASD before two years old had received early screening, while only 17.61% of the children diagnosed with ASD after two years old had received early screening (72). Also, children with ASD who received an early diagnosis before two years had higher levels of adaptive behavior, personal and social development, and self-help ability than those who received a diagnosis after 2 (72). Furthermore, when comparing the diagnostic age of ASD children in the community early screening group with that in the voluntary visit group, Li et al. reported that children in the community early screening group received a diagnosis 15 months earlier, and the early intervention rate in the community early screening group was 85.71% (27).
At present, while early screening for ASD has been carried out in many areas of China, the results of screening in some areas are not satisfactory due to the lack of proper management and standardized procedures. Early screening of ASD has not been widely promoted in the child healthcare system. The standardized screening process should be improved, and continuous quality management and monitoring should be carried out, according to the specific conditions of different regions. Also, ASD early screening should be integrated into the routine work of child health care in the three-level child healthcare system to normalize and standardize ASD early screening.
Conclusions
Despite a late start with ASD clinical diagnosis and treatment research and clinical services in China, with the continuous improvement of community ASD work and increasing attention for ASD, early screening and diagnosis techniques have been developed in some provinces and communities. ASD clinical diagnosis and treatment achievements in China provide a reference for other regions, even the whole country, to implement national ASD clinical diagnosis and treatment programs. Further program improvements are still required. In the future studies, there is a need to further explore a set of ASD early screening tools and diagnostic screening procedures suitable for China’s national conditions, with the hope of providing an opportunity for more ASD children to get early intervention.
Acknowledgments
Funding: This work supported by the National Key Research and Development Program of China [grant numbers 2016YFC1306205]; National Natural Science Foundation of China [grant numbers 61733011].
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Geraldine Dawson and Lauren Franz) for the series “Implementing Autism Early Intervention: A Global Perspective” published in Pediatric Medicine. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/pm.2019.07.01). The series “Implementing Autism Early Intervention: A Global Perspective” was commissioned by the editorial office without any funding or sponsorship. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM 5). ed 5th ed., Washington, DC, American Psychiatric Publishing, 2013.
- Kanner L. Autistic disturbances of affective contact. Nervous Child 1943;2:217-50.
- Baio J, Wiggins L, Christensen DL, et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. Mmwr Surveill Summ 2018;67:1-23. [Crossref] [PubMed]
- Lai MC, Lombardo MV, Baron-Cohen S, et al. Autism. Lancet 2014;383:896-910. [Crossref] [PubMed]
- Wang Y, Wang W, Yan D, et al. Application of Early Screening Model of Lonely Spectrum Disorder in Child Health Service System Chin J Child Health Care 2014;5:921-4. (in Chinese).
- Jiang L, Li G, Hao L, et al. Epidemiological investigation on autism spectrum disorders among preschool children in Shanghai Zhonghua Liu Xing Bing Xue Za Zhi 2015;36:1365-8. (in Chinese). [PubMed]
- Sun X, Allison C, Wei L, et al. Autism prevalence in China is comparable to Western prevalence. Mol Autism 2019;10:7. [Crossref] [PubMed]
- China NMOH: China sample survey of disabled children aged 0-6. Beijing, China Statistics Press, 2003.
- Bhat S, Acharya UR, Adeli H, et al. Autism: cause factors, early diagnosis and therapies. Rev Neurosci 2014;25:841-50. [Crossref] [PubMed]
- Xu X. Early Screening and Diagnosis of Children's Autism Spectrum Disorder. Chin J Prac Pediatr 2013;8:576-9.
- Lavelle TA, Weinstein MC, Newhouse JP, et al. Economic burden of childhood autism spectrum disorders. Pediatrics 2014;133:e520-9. [Crossref] [PubMed]
- Shimabukuro TT, Grosse SD, Rice C, et al. Medical expenditures for children with an autism spectrum disorder in a privately insured population. J Autism Dev Disord 2008;38:546-52. [Crossref] [PubMed]
- Xu Z, Wang J, Sun X, et al. Current status of family economic burden of children with autism spectrum disorder in Heilongjiang Province (in Chinese). Chin J School Health 2018;39:335-37, 342.
- Zwaigenbaum L, Bauman ML, Stone WL, et al. Early Identification of Autism Spectrum Disorder: Recommendations for Practice and Research. Pediatrics 2015;136:S10-40. [Crossref] [PubMed]
- Association DBGO, Committee CMAP, Project EGOC, et al. Expert Consensus on Early Identification Screening and Intervention for Children with ASD Chin J Pediatr 2017;55:890-97. (in Chinese).
- Schreibman L, Dawson G, Stahmer AC, et al. Naturalistic Developmental Behavioral Interventions: Empirically Validated Treatments for Autism Spectrum Disorder. J Autism Dev Disord 2015;45:2411-28. [Crossref] [PubMed]
- Dawson G, Rogers S, Munson J, et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics 2010;125:e17-23. [Crossref] [PubMed]
- Wingate M, Kirby RS, Pettygrove S, et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2010. MMWR Surveill Summ 2014;63:1-21. [PubMed]
- Noland RM, Gabriels RL, et al. Screening and identifying children with autism spectrum disorders in the public school system: the development of a model process. J Autism Dev Disord 2004;34:265-77. [Crossref] [PubMed]
- Robins DL, et al. Screening for autism spectrum disorders in primary care settings. Autism 2008;12:537-56. [Crossref] [PubMed]
- Chlebowski C, Robins DL, Barton ML, et al. Large-scale use of the modified checklist for autism in low-risk toddlers. Pediatrics 2013;131:e1121-7. [Crossref] [PubMed]
- Johnson CP, Myers SM, et al. Identification and evaluation of children with autism spectrum disorders. Pediatrics 2007;120:1183-215. [Crossref] [PubMed]
- Tao G. Diagnosis and attribution of autism in infants Chin J Psychiatry 1982;2:104-7. (in Chinese).
- Zwaigenbaum L, Bauman ML, Choueiri R, et al. Early Identification and Interventions for Autism Spectrum Disorder: Executive Summary. Pediatrics 2015;136:S1-9. [Crossref] [PubMed]
- Rotholz DA, Kinsman AM, Lacy KK, et al. Improving Early Identification and Intervention for Children at Risk for Autism Spectrum Disorder. Pediatrics 2017;139: [Crossref] [PubMed]
- Huang XN, Zhang Y, Feng W, et al. Reliability and validity of warning signs checklist for screening psychological, behavioral and developmental problems of children. Zhonghua Er Ke Za Zhi 2017;55:445-50. [PubMed]
- Li C, Zhu G, Feng J, et al. Improving the early screening procedure for autism spectrum disorder in young children: Experience from a community-based model in shanghai. Autism Res 2018;11:1206-17. [Crossref] [PubMed]
- Baron-Cohen S, Allen J, Gillberg C, et al. Can autism be detected at 18 months? The needle, the haystack, and the CHAT. Br J Psychiatry 1992;161:839-43. [Crossref] [PubMed]
- Robins DL, Fein D, Barton ML, et al. The Modified Checklist for Autism in Toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. J Autism Dev Disord 2001;31:131-44. [Crossref] [PubMed]
- Robins DL, Casagrande K, Barton M, et al. Validation of the modified checklist for Autism in toddlers, revised with follow-up (M-CHAT-R/F). Pediatrics 2014;133:37-45. [Crossref] [PubMed]
- Gong Y, Liu J, Li C, et al. Reliability and validity of the Chinese version of the Modified Checklist for Autism in Toddlers Chin Ment Health J 2011;25:409-14. (in Chinese).
- Gong Y, Liu J, Li C, et al. Reliability and validity of the Chinese revised version of the Modified Checklist for Autism in Toddlers Chin Ment Health J 2012;26:476-80. (in Chinese).
- Gong Y, Liu J, Guo Y, et al. Validity and reliability of the Chinese simplified version of the Modified Checklist for Autism in Toddlers Chin Ment Health J 2015;29:121-4. (in Chinese).
- Luo M, Gou C, Cao M, et al. Efficacy evaluation of autism screening in toddlers by using the M-CHAT-R/F combined with Ages and Stages Questionnaire Chin J Child Health Care 2018;26:262-5. (in Chinese).
- Wong V, Hui LS, Lee W, et al. A Modified Screening Tool for Autism (Checklist for Autism in Toddlers [CHAT-23]) for Chinese Children. Pediatrics 2004;114:e166-76. [Crossref] [PubMed]
- Wu F: Applied research on autism screening scale(in Chinese). In, Fudan University, 2009.
- Clancy H, Dugdale A, Rendle-Short J, et al. The diagnosis of infantile autism. Dev Med Child Neurol 1969;11:432-42. [Crossref] [PubMed]
- Sun X, Allison C, Auyeung B, et al. Comparison between a Mandarin Chinese version of the Childhood Autism Spectrum Test and the Clancy Autism Behaviour Scale in mainland China. Res Dev Disabil 2014;35:1599-608. [Crossref] [PubMed]
- Ke X, Luo S, Tao G, et al. A Study of Clancy Behavior Scale on Childhood Autism Acta Academiae Medicinae Jiangxi 2002;42:136-7. (in Chinese).
- Chen Y, Chen Z, Zhuo R, et al. Clinical application of Clancy autism behavior scale Guangdong Med J 2007;28:375-77. (in Chinese).
- Goldstein S NJ: Autism spectrum rating scales (ASRS™). Tonawanda, NY, Multi-Health Systems, 2009.
- Zhou H, Zhang L, Yan W, et al. Construct validity of the Autism Spectrum Rating Scale of the Revised Chinese Version. Chin J Contemp Pediatr 2015;230:1282-85. [PubMed]
- Zhou H, Zhang L, Luo X, et al. Modifying the Autism Spectrum Rating Scale (6-18 years) to a Chinese Context: An Exploratory Factor Analysis. Neurosci Bull 2017;33:175-82. [Crossref] [PubMed]
- Zhou H, Zhang L, Wu L, et al. Validity and reliability analysis of the Chinese parent version of the Autism Spectrum Rating Scale (6-18 years). Psychiatry Res 2015;230:255-61. [Crossref] [PubMed]
- Zhou H, Zhang L, Zou X, et al. Chinese Norms for the Autism Spectrum Rating Scale. Neurosci Bull 2017;33:161-7. [Crossref] [PubMed]
- Liu J, Wang Y, Guo Y, et al. The Development of a Screening Checklist for Childhood Autism. Chin Ment Health J 2004;6:400-3.
- Krug DA, Arick J, Almond P, et al. Behavior checklist for identifying severely handicapped individuals with high levels of autistic behavior. J Child Psychol Psychiatry 1980;21:221-9. [Crossref] [PubMed]
- Yang X, Huang Y, Jia M, et al. Autism Behavior Scale Test Report (in Chinese). Chin Ment Health J 1993;6:279-80, 275.
- Ai-Yue LI, Xin Z, Cong-Chao LV, et al. Analysis of behavioral characteristics of children with autism aged 1.5~3 years old. Chin Ment Health J 2010;24:215-8.
- Li J, Cai L, Zhong J, et al. Assessment of 32 Children with Autism by Autism Behavior Scale. Pract Clin Med 2002;3:3.
- Rellini E, Tortolani D, Trillo S, et al. Childhood Autism Rating Scale (CARS) and Autism Behavior Checklist (ABC) correspondence and conflicts with DSM-IV criteria in diagnosis of autism. J Autism Dev Disord 2004;34:703-8. [Crossref] [PubMed]
- Snow AV, Lecavalier L, et al. Sensitivity and specificity of the Modified Checklist for Autism in Toddlers and the Social Communication Questionnaire in preschoolers suspected of having pervasive developmental disorders. Autism 2008;12:627-44. [Crossref] [PubMed]
- Liu J: Early screening of autism spectrum disorders and clinical data of children with autism(in Chinese). In, Fudan University, 2011:55.
- Schopler E, Reichler RJ, DeVellis RF, et al. Toward objective classification of childhood autism: Childhood Autism Rating Scale (CARS). J Autism Dev Disord 1980;10:91-103. [Crossref] [PubMed]
- Li J, Zhong J, Cai L, et al. Clinical application study of childhood autism assessment scale Chin J Child Health Care 2005;13:267-68. (in Chinese).
- Gotham K, Risi S, Pickles A, et al. The Autism Diagnostic Observation Schedule: revised algorithms for improved diagnostic validity. J Autism Dev Disord 2007;37:613-27. [Crossref] [PubMed]
- Luyster R, Gotham K, Guthrie W, et al. The Autism Diagnostic Observation Schedule-toddler module: a new module of a standardized diagnostic measure for autism spectrum disorders. J Autism Dev Disord 2009;39:1305-20. [Crossref] [PubMed]
- Zhou B, Xu Q, Lu P, et al. Evaluation on reliability and validity of Chinese version Autism Diagnostic Observation Schedule Module-1 and clinical application Chin J Evid Based Pediatr 2013;8:257-61. (in Chinese).
- Saemundsen E, Magnusson P, Smari J, et al. Autism Diagnostic Interview-Revised and the Childhood Autism Rating Scale: convergence and discrepancy in diagnosing autism. J Autism Dev Disord 2003;33:319-28. [Crossref] [PubMed]
- Guo Y, Yang X, Liu J, et al. Reliability and diagnostic validity study on Autism Diagnostic Interview-Revised Chin J Psychiatry 2002;35:42-5. (in Chinese).
- Mao M, Jiang F, et al. Historical development and challenges of the child health care in China. Zhonghua Er Ke Za Zhi 2011;49:325-8. [PubMed]
- Wei Z, Ren L, Weng L, et al. Screening of autism spectrum disorder in infants aged 18~24 months in Shenzhen and 3-year follow-up study Chin J Child Health Care 2012;20:354-7. (in Chinese).
- Wang Y, Wang W, et al. Application analysis of DSM-V in early screening of children with autism spectrum disorder Matern Child Health Care China 2015;13:2011-14. (in Chinese).
- Huang JP, Cui SS, Han Y, et al. Prevalence and early signs of autism spectrum disorder (ASD) among 18-36 month-old children of Tianjin in China. Biomed Environ Sci 2014;27:453-61. [PubMed]
- Li Q, Wang P, Cao Y, et al. Early screening of infants with autism and its influencing factors J Occup Health 2015;17:2434-36. (in Chinese).
- Yu Q, Sun X. Effect evaluation of community monitoring model for children with autism spectrum disorder Chin Matern Child Health Res 2016;9:1069-70. (in Chinese).
- Guo W, Zhu G, Zhou Z, et al. Application study of Chat-23 scale in screening early childhood autism in the community Matern Child Health Care China 2013;28:5308-11. (in Chinese).
- Lv L, Qian Y, Hu Y, et al. Early screening management model for children with autism spectrum disorder Chin J Child Heal Care 2015;23:1313-5. (in Chinese).
- Xie Y, Xie X, Zheng X, et al. Study on community screening management model for early diagnosis of autism spectrum disorder in children Matern Child Health Care China 2012;19:2904-06. (in Chinese).
- Reichow B, Barton EE, Boyd BA, et al. Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD). Cochrane Database Syst Rev 2012;10:CD009260 [PubMed]
- Dawson G, Jones EJ, Merkle K, et al. Early behavioral intervention is associated with normalized brain activity in young children with autism. J Am Acad Child Adolesc Psychiatry 2012;51:1150-59. [Crossref] [PubMed]
- Huang S, Lin Y, Wei Z, et al. Analysis of influencing factors in early diagnosis of autism spectrum disorder Chin J Child Health Care 2018;4:407-11. (in Chinese).
Cite this article as: Li C, Xu X. Early screening and diagnosis for ASD children in China. Pediatr Med 2019;2:35.