Approaches to the thoracic cavities
Introduction
In the past, the posterolateral thoracotomy was utilized as the usual incision in pediatric patients. Nevertheless, in children, most thoracotomic operations could be performed through a muscle sparing lateral thoracotomy. The video-assisted thoracic surgery (VATS) is progressively more used since most procedures can be tailored to VATS. On the contrary, median sternotomy has a partial role and consent the access to both lungs and mediastinal structures (1).
Thoracotomic incisions
Posterolateral thoracotomy
The posterolateral thoracotomy provides excellent access to:
- Lung;
- Oesophagus;
- Mediastinum;
- Descending aorta;
- Diaphragm.
The standard incision extends:
- From the anterior axillary line;
- To a point midway between the vertebral border of the scapula and the spine (level of the fourth thoracic vertebra);
- The incision may be extended anteriorly or posteriorly.
Steps:
- Division of the trapezius muscles and latissimus dorsi;
- Elevation and anterior retraction of the serratus anterior muscle;
- Division of the serratus anterior muscle origins from the underlying ribs;
- Preservation of the neurovascular bundle to avoid the winging of the scapula;
- Thorax is opened through the bed of the fifth intercostal space;
- Identification of the parietal pleura.
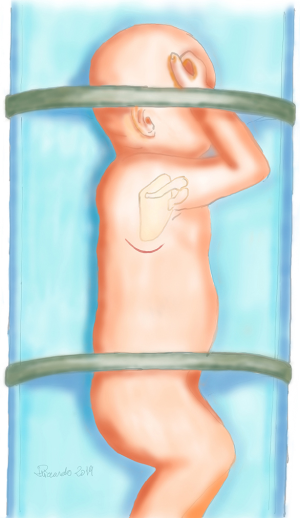
If an extrapleural approach is intended, the pleura is gently separated from the inside of the chest wall using small damp gauze or can also be opened through the bed of a rib. The posterior periosteum can be opened to gain entry to the thoracic cavity. In the case of complexity, broader access could be achieved removing the whole bone or excising a segment of the posterior rib (Figure 1).
Lateral and auscultatory triangle muscle-sparing thoracotomies
The general principle of muscle-sparing thoracotomies is retraction rather than the division of the chest wall muscles.
The skin incision runs:
- From the anterior axillary line;
- To a point midway between the vertebral border of the scapula and the spine, at the level of the fourth thoracic vertebra.
Steps:
- Undermine the anterior and anteroinferior edges of the wound;
- Exposition of the latissimus dorsi and serratus anterior muscles;
- Definition of the anterior boundary of the latissimus dorsi muscle;
- Posterior retraction of the muscle to expose the serratus anterior.
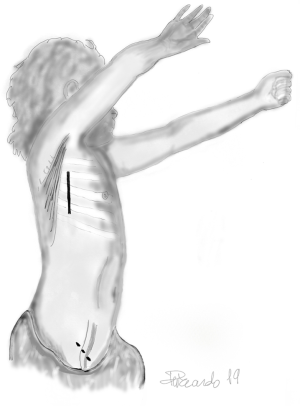
Further retraction of the latissimus dorsi to delineate the posterior border of the serratus anterior (Figure 2) (2-4).
The muscle-sparing technique can also be used to enter the chest through the triangle of auscultation (trapezius superiorly, the posterior border of latissimus dorsi inferiorly, and the vertebral border of the scapula laterally).
The skin incision for auscultatory triangle muscle-sparing thoracotomies:
- Slightly more posteriorly than for a lateral thoracotomy (5).
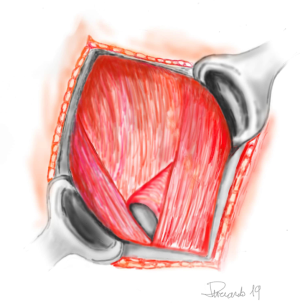
The lateral incision offers a little less exposure than the usual posterolateral thoracotomy but is quite acceptable if completed with the proper mobilization of the latissimus dorsi and complete exposure of the intercostal space (Figure 3) (4).
Muscle sparing posterolateral thoracotomy
The skin incision is the same as posterolateral thoracotomy. The anterior margin is generally found between the posterior axillary fold and the anterior superior iliac spine, although the latissimus dorsi inserts on the posterior aspect of the iliac crest.
A slightly longer skin incision is required to realize an adequate muscle flap. The subcutaneous attachments of the latissimus dorsi are prepared. The entire anterior border is freed inferiorly toward the iliac crest and superiorly into the axilla. The profound margin of the latissimus dorsi is released. The muscle is retracted posteriorly, exposing the serratus anterior that is dissected by dividing the fascia along the posterior margin up to the tip of the scapula, down to the lowest attachment on the anterior aspect of the sixth rib. The profound element of the serratus is mobilized, retracting the muscle forward. The bones are viewed for choosing the entry level into the pleura (6,7).
Transaxillary thoracotomy
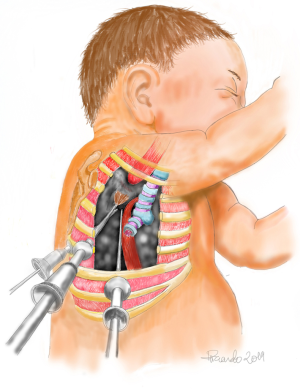
The skin incision could be vertical or horizontal. To expose the serratus anterior, the subcutaneous tissue and fascia are divided. Tissue planes are developed between the superficial fascia. The muscle layers should be taken care to avoid the long thoracic and the intercostobrachial nerves. Latissimus dorsi is retracted posteriorly, elevating the serratus anterior muscle, and exposing the desired rib space. The third intercostal space is best suited for operations on the patent ductus arteriosus, sympathetic chain, and apical lung lesions. The fourth space is used for biopsy of mediastinal lesions, upper lobectomy pleurodesis, and wedge resection (Figure 4) (6-8).
Minimally-invasive thoracic surgery approaches
Minimal access thoracic surgery carries with it several concerns, including aesthetic considerations, control of vascular structures, and adequate workspace. Advances in new generation products including shorter instruments, high-resolution cameras, improved linear staplers and endoclip, energy devices, have further popularized VATS in children. The breadth of minimally invasive indication was shown in Table 1. The most common indications include pleural debridement for empyema, the mediastinal lesions biopsy and excision of duplication or bronchogenic cysts. The VATS is useful for other pleural disorders, such as chylothorax and spontaneous pneumothorax. Latest developments are being created to performing anatomic lobectomies, repair of oesophageal atresia and diaphragmatic hernias (Figure 5). The role of the robot in pediatric thoracoscopy is still in the preliminary stages of definition (9,10).
Table 1
| Cyst excision |
| Decortication |
| Excision of the mediastinal mass |
| Ligation of ductus arteriosus |
| Ligation of the thoracic duct |
| Lobectomy |
| Lung biopsy |
| Mediastinal biopsy |
| Pericardial window |
| Pleurectomy |
| Plication of diaphragm |
| Repair of a diaphragmatic hernia |
| Repair of oesophageal atresia |
| Repair of tracheoesophageal fistula |
| Resection of foregut duplication |
| Resection of sequestration |
| Sympathectomy |
| Thymectomy |
VATS, video-assisted thoracic surgery.
Acknowledgments
Authors give a special thanks to Eng. Riccardo Pardolesi who helped and contributed to this paper with his fabulous original pictures.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Paolo Scanagatta) for the series “Pediatric Thoracic Surgery” published in Pediatric Medicine. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/pm.2019.03.06). The series "Pediatric Thoracic Surgery" was commissioned by the editorial office without any funding or sponsorship. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Parikh DH, Crabbe DC. Thoracic Incisions and Operative Approaches. In: Parikh DH, Crabbe DC, Auldist AW, et al. (eds). London: Pediatric Thoracic Surgery Springer, 2009;81-92.
- Findik G, Gezer S, Sirmali M, et al. Thoracotomies in children. Pediatr Surg Int 2008;24:721-5. [Crossref] [PubMed]
- Heitmiller RF. The serratus sling: a simplified serratus-sparing technique. Ann Thorac Surg 1989;48:867-8. [Crossref] [PubMed]
- Mitchell R, Angell W, Wuerflein R, et al. Simplified lateral chest incision for most thoracotomies other than sternotomy. Ann Thorac Surg 1976;22:284-6. [Crossref] [PubMed]
- Kittle CF. Which way in?--The thoracotomy incision. Ann Thorac Surg 1988;45:234. [Crossref] [PubMed]
- Becker RM, Munro DD. Transaxillary minithoracotomy: the optimal approach for certain pulmonary and mediastinal lesions. Ann Thorac Surg 1976;22:254-9. [Crossref] [PubMed]
- Massimiano P, Ponn RB, Toole AL. Transaxillary thoracotomy revisited. Ann Thorac Surg 1988;45:559-60. [Crossref] [PubMed]
- Durkovic S, Scanagatta P. Muscle-Sparing Thoracotomy: A Systematic Literature Review and the “AVE” Classification. J Surg Surgical Res 2015;1:35-44.
- Engum SA. Minimal access thoracic surgery in the pediatric population. Semin Pediatr Surg 2007;16:14-26. [Crossref] [PubMed]
- Kugler C. Minimal-invasive thoracic surgery in pediatric patients. J Vis Surg 2018;4:10. [Crossref] [PubMed]
Cite this article as: Bertolaccini L, Pardolesi A. Approaches to the thoracic cavities. Pediatr Med 2019;2:9.